ANN ONCOL :生物标记物:识别肿瘤侵袭!
2017-07-27 佚名 来宝网
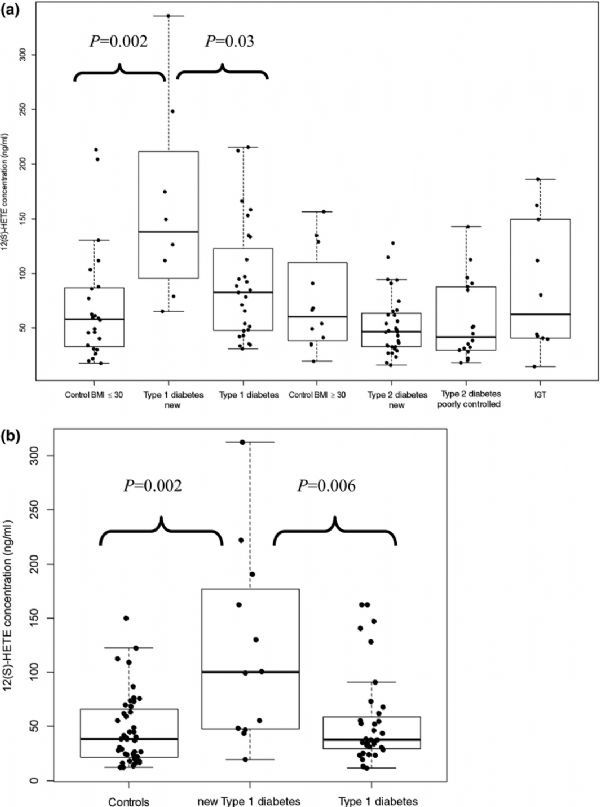
早期结肠癌患者将来可以从特定额基因测试中获益,并帮助他们在化疗方面做出正确的决定。其中两种生物标记物是MACC1基因,高水平促进肿瘤的生长和肿瘤的转移,以及一种有缺陷的DNA不匹配修复(dMMR)系统,它在肿瘤的形成中起着重要的作用。患有dMMR肿瘤和低MACC1基因活性的患者的预期寿命更长。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#标记物#
31
#Oncol#
0
#生物标记#
22
#生物标记物#
34
学习了,谢谢分享
51
谢谢分享。
48
在一项大约600 位第二阶段结肠癌患者(局部侵略性肿瘤没有转移)的研究中,第一次显示MACC1基因测试可以帮助进一步区分有缺陷的修复机制。对于那些有缺陷的修复机制的患者来说,这种预后是积极的:100%的5年生存率。基因检测也可能对推荐的治疗方法有影响。
44
学习谢谢分享
54
学习学习学习
58
谢谢分享,学习了
19