JASN:糖尿病肾病的新生物标记物
2017-05-08 MedSci medicalxpress
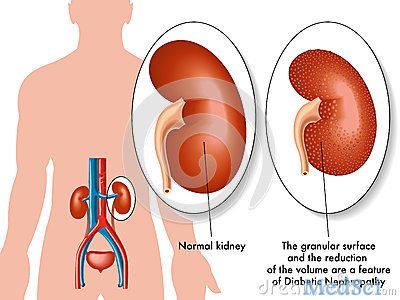
2型糖尿病的常见并发症发生在肾小球的过滤作用受损时,导致尿液中蛋白质的异常积累和肾功能的下降。这种称为糖尿病肾病的病症可能导致目前难以预测的不可逆的肾衰竭。西奈山的伊坎健康学院医学教授Chirag Parikh领导的研究小组进行了一项研究最近取得了进展,这将有助于改善这种疾病的诊断和治疗方案。
2型糖尿病的常见并发症发生在肾小球的过滤作用受损时,导致尿液中蛋白质的异常积累和肾功能的下降。这种称为糖尿病肾病的病症可能导致目前难以预测的不可逆的肾衰竭。西奈山的伊坎健康学院医学教授Chirag Parikh领导的研究小组进行了一项研究最近取得了进展,这将有助于改善这种疾病的诊断和治疗方案。
为了评估这些生物标记物,该研究小组进行了早期随机对照试验,控制糖尿病心血管危险行动研究(ACCORD)和晚期退伍军人糖尿病实验研究(VANEPHRON-D)。测量了来自两个大型联邦资助临床试验样本中糖尿病患者血液中的三种特异性蛋白(TNFR-1,TNFR-2和KIM-1)。他们测试这些蛋白质是否与肾脏滤过功能的下降有关。
结果显示,在基线水平时,NEPHRON-D晚期糖尿病肾病(DKD)人群的TNFR-1,TNFR-2和KIM-1的中位浓度比ACCORD早期DKD人群的浓度大约高出两倍。在两项研究中,到达肾病的患者的基线水平高于那些没有达到这个结果的患者。TNFR-1,TNFR-2和KIM-1水平翻倍与肾病风险之间的关系在两组研究中都具有显着差异。在NEPHRON-D的临床中,将这些生物标记物纳入临床模型中,肾病变率从0.68(0.02)增加到0.75(0.02)。此外,系统的文献综述表明在DKD中,这些炎症因子和肾病变之间高度相关。与早期和晚期糖尿病肾病患者相比,每种蛋白质与肾功能下降的风险独立相关。
这些结果显示,这些蛋白质作为生物标志物在预测糖尿病患者肾脏疾病进展的方面以及评估疾病治疗在临床试验中的功效具有潜在作用。
原文出处:Steven G. Coca et al. Plasma Biomarkers and Kidney Function Decline in Early and Established Diabetic Kidney Disease, Journal of the American Society of Nephrology (2017).
此文系梅斯医学(MedSci)原创编译整理,转载须授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#标记物#
35
#ASN#
38
#生物标记#
35
#生物标记物#
28