JAMA Oncol:仿制药HD201在ERBB2阳性乳腺癌中的疗效堪比曲妥珠单抗!
2022-03-11 Nebula MedSci原创
曲妥珠单抗的使用改变了ERBB2阳性乳腺癌的治疗和预后。但是,曲妥珠单抗的高昂费用限制了很多患者的使用。通过开发类似曲妥珠单抗的生物仿制药或有助于满足大量乳腺癌患者的需求。
曲妥珠单抗的使用改变了ERBB2阳性乳腺癌的治疗和预后。但是,曲妥珠单抗的高昂费用限制了很多患者的使用。通过开发类似曲妥珠单抗的生物仿制药或有助于满足大量乳腺癌患者的需求。
HD201是新加坡Prestige BioPharma Ltd开发的曲妥珠单抗的生物仿制药。本研究旨在对比HD201与曲妥珠单抗在ERBB2阳性乳腺癌患者中的效果。
这是一项在12个国家的70家医疗中心开展的随机的临床试验(TROIKA),共招募了502位明确诊断的ERBB2阳性的早期乳腺癌,随机分成两组,接受HD201或曲妥珠单抗治疗8个疗程,所有患者同时接受4个疗程的多西紫杉醇,继以4个疗程的表柔比星和环磷酰胺,然后接受手术治疗;术后,患者再接受10个疗程的HD201或曲妥珠单抗治疗。主要终点是总的病理完全缓解率。次要终点包括乳腺病理完全缓解率、总缓解率、无事件生存率、总生存率、安全性、药代动力学和免疫学。
502位女性患者(平均53岁)随机接受了HD201或曲妥珠单抗治疗,其中474位(94.2%)符合分析纳入标准。两组受试患者的基线特征均衡良好;195例(38.8%)肿瘤是激素受体阴性,213例(42.4%)为临床3期。
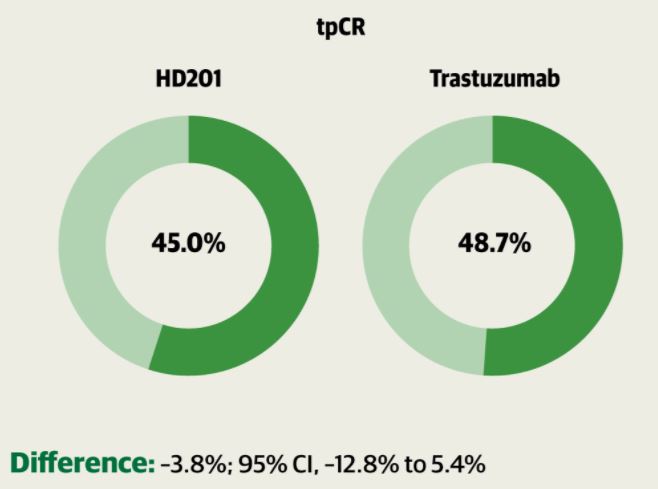
两组的总病理完全缓解率
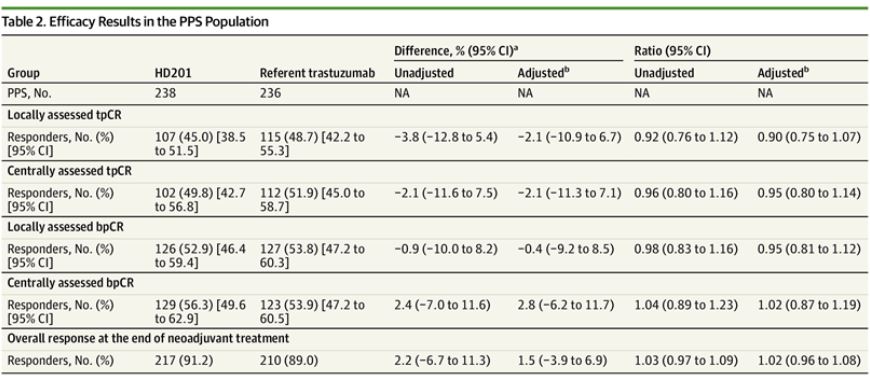
HD201组和曲妥珠单抗组的总病理完全缓解率分别是45%和48.7%,两组的差值为-3.8%,无显著性。两组的总病理完全缓解率的比值是0.92。在整个治疗过程中,433位(86.1%)患者共发生了2232例需紧急治疗的不良事件,HD201组和曲妥珠单抗组的发生率分别是88.0%和84.5%。
意向治疗人群的疗效分析
总之,该随机试验表明,HD201用于治疗ERBB2阳性乳腺癌的疗效堪比曲妥珠单抗。这对于广大乳腺癌患者而言,值得奔走相告。
原始出处:
Xavier Pivot, et al. Efficacy of HD201 vs Referent Trastuzumab in Patients With ERBB2-Positive Breast Cancer Treated in the Neoadjuvant Setting A Multicenter Phase 3 Randomized Clinical Trial. JAMA Oncol. Published online March 3, 2022. doi:10.1001/jamaoncol.2021.8171
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Oncol#
57
#曲妥珠#
46
#ErbB2#
54
#仿制药#
40