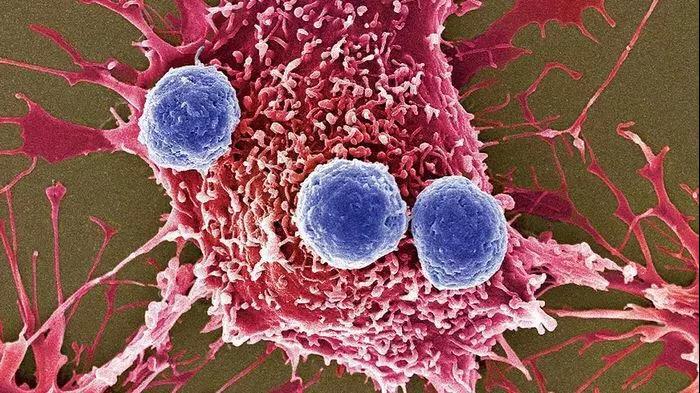
实体瘤患者PD-L1表达与TMB、MSI的相关性研究
2019-06-12 蔡修宇 肿瘤资讯
在今年ASCO会议上,中山大学附属肿瘤医院蔡修宇教授报道了一项中国实体瘤患者PD-L1表达水平与TMB、MSI的相关性研究。自2018年4月9日至2018年12月26日,共入组了197位实体瘤患者,包含了包括肺癌、结直肠癌、胃癌等18种癌症。收集所有患者的新鲜肿瘤组织或FFPE样本,对所有的样本进行靶向测序(包含605个基因),分析计算TMB,利用免疫组化检测分析PD-L1的表达,此外采取多重荧光
研究结果
197例实体瘤患者中,18.78%(37/197例)的患者PD-L1在肿瘤细胞中高表达(≥50%),74.11%(146/197例)的患者低表达(1%~49%);5.08%(10/197例)的患者为微卫星不稳定高表达(MSI-H);4.06%(8/197例)的患者为高TMB(>20 Muts/Mb),29.44%(58/197例)的患者为中TMB(>6且≤ 20Muts/Mb)。其中37例PD-L1高表达的患者中,仅有1例为TMB-H,3例为MSI-H。而在PD-L1表达阴性(<1%)的患者中,57.14%(8/14例)的患者为TMB-H或者MSI-H(3例仅TMB-H,3例仅MSI-H,2例为TMB-H且MSI-H)。在10例MSI-H的患者中,有4例为TMB-H。
研究结论
从初步的研究结果可知,在实体瘤患者中PD-L1表达水平与TMB、MSI存在一定相关性, PD-L1表达阴性的患者为TMB-H或MSI-H的概率高于PD-L1表达阳性的患者,MSI-H与TMB-H呈正相关。
在一项十万人测序研究中,Foundation Medicine比较了TMB和MSI-H之间的关系,样本来自其中同时拥有TMB和MSI数据的6万多个患者样本数据,结果发现在MSI-H的患者中,97%的患者TMB不小于10 Muts/Mb,83%的患者不小于20 Muts/Mb,反之,只有16%的高TMB的患者为MSI高度不稳定,所以MSI-H可能是导致高TMB的一个因素。可以将MSI-H理解为高TMB的一个子集,绝大多数MSI-H的患者都为高TMB,但高TMB的患者,并非都是MSI不稳定型,还有相当一部分患者是MSI稳定型。我们的研究结果与本研究一致。
2018年,MSK对240例接受PD-1抑制剂治疗的晚期肺癌患者的相关资料进行总结和分析时,发现PD-L1表达高低和TMB高低无关。PD-L1表达量低的,TMB不一定低;TMB低的,可能PD-L1表达是高的。PD-L1表达量和TMB同时都高的患者,疗效最好,临床获益率为50%;两者都低的患者,使用PD-1抑制剂,临床获益率只有18.2%。TMB与PD-L1表达是两个独立的生物标志物。此外Checkmate 026研究也能很好说明TMB与PD-L1表达是两者独立的生物标志物,在PD-L1表达>5%的NSCLC患者中,Opdivo相比化疗,PFS(4.2 vs 5.9个月)和OS(14.4 vs 13.2个月)都没有显着提高,宣告实验失败。但在回顾性研究中发现,相比PD-L1表达,TMB能很好地区分免疫获益人群。我们的研究结果和MSK的这项研究结果不一致,需要更大样本来探究PD-L1表达水平和TMB及MSI的关系。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TMB#
44
#PD-L1表达#
43
#相关性#
31
#PD-L1#
40
#MSI#
48
学习了,谢谢分享
67