Lancet:低温导致心脏骤停6小时后神经功还能完全恢复?
2020-07-19 杨中华 脑血管病及重症文献导读
34岁,女性。在西班牙北部的一次登山旅行中倒下,最初在一个救援中心接受了评估。
34岁,女性。在西班牙北部的一次登山旅行中倒下,最初在一个救援中心接受了评估。
患者无反应,心跳停止,无脉搏,瞳孔散大无反应,鼓膜温度为18°C。
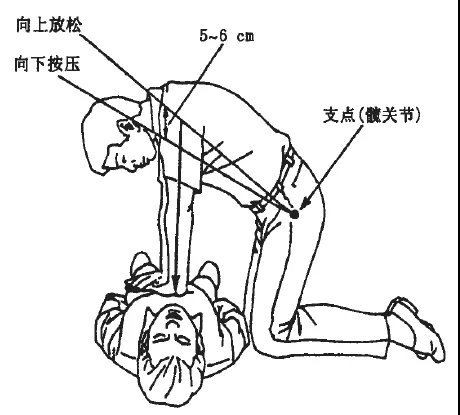
开始高级生命支持,被转移到我们医院。
第一次评估后2小时25分钟,她仍然处于心脏停搏状态,瞳孔散大无反应,核心温度为20.2°C。动脉血样显示pH值为6.81,乳酸浓度为10.3 mmol/L(正常值为0.5–1),钾浓度为4.4 mmol/L(正常值为3.5–5)。
开始外周静脉动脉ECMO支持,ECG立即显示心室颤动。病人也开始喘息,并出现呼吸机不同步,双谱指数监护仪显示爆发抑制;给予镇静剂后消失。
在体外支持的最初几个小时内,患者出现凝血障碍、出血、肺水肿和ECMO流量的异常。然而,患者稳定下来后,她的体温以每小时3°C的速度逐渐升高。患者在体外支持3小时后恢复瞳孔反应。当体温达到30℃时,可观察到粗大的心室颤动。然后对她进行了除颤,产生了有效节律,这意味着在初次评估后6小时10分钟,恢复了自主循环。当体温达到32°C时,心电图显示窦性心律伴有经典的Osborn或J波,在V3导联中清晰可见。在重症监护病房(ICU)的第1天,患者的神经元特异性烯醇化酶为93.4 ng/mL(正常范围1.5-13.5);第2天,降至55.1 ng/mL;其他实验室检查在患者恢复期间逐渐正常。
继续升温直至患者体温为35℃。在45小时40分钟后停止ECMO。患者在ICU停留的第2天成功拔管。
第2天结束时的神经学评估未发现异常,第6天转出ICU。第11天回家。发作一个月后,她恢复了正常的日常生活活动。
长时间心脏骤停后神经系统后遗症很常见。维持体外支持和神经保护以及体温管理,直到恢复足够的双心室功能(如我们的情况)可能是预防脑损伤的关键。该患者的体外支持总共45小时40分钟,这比先前报道的时间长得多。在低体温和心搏停止的情况下,应考虑使用ECMO作为氧气重新分配和温度管理手段进行复苏。
原始出处:Jordi Riera, Eduard Argudo, Juan Carlos Ruiz-Rodríguez, et al. Full Neurological Recovery 6 H After Cardiac Arrest Due to Accidental Hypothermia. Lancet. 2020 May 16.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Lancet#
27
学习了
87
#心脏骤停#
202
#低温#
134
顶刊就是不一样,质量很高,内容精彩!学到很多
49