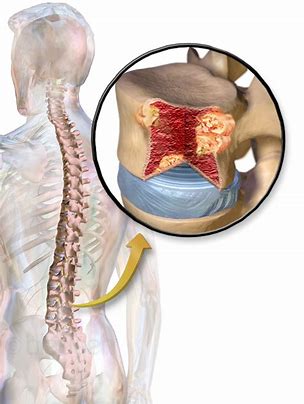
抗BCMA药物belantamab mafodotin治疗多发性骨髓瘤的关键研究达到主要终点
2019-08-26 Allan MedSci原创
葛兰素史克近日宣布,实验性药物belantamab mafodotin治疗复发/难治多发性骨髓瘤患者的关键性研究(DREAMM-2试验)符合其主要终点,患者对belantamab mafodotin的总体反应率(ORR)较高。
葛兰素史克近日宣布,实验性药物belantamab mafodotin治疗复发/难治多发性骨髓瘤患者的关键性研究(DREAMM-2试验)符合其主要终点,患者对belantamab mafodotin的总体反应率(ORR)较高。
Belantamab mafodotin,也称为GSK2857916,是一种免疫缀合物,其包含人源化抗BCMA单克隆抗体、接头和细胞毒性剂auristatin F。药物接头技术由Seattle Genetics许可。今年早些时候,GlaxoSmithKline报道了DREAMM-1研究的最新结果,证实了复发/难治多发性骨髓瘤患者对belantamab mafodotin的ORR为60%。
原始出处:
http://www.firstwordpharma.com/node/1661304?tsid=4#axzz5xf7rqWhf
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#多发性#
20
#主要终点#
37
#mAb#
29
#抗BCMA#
57
#BCMA#
26
学习了,谢谢分享
70