Eur Heart J:房颤消融术后患者的并发症评估
2017-01-23 MedSci MedSci原创
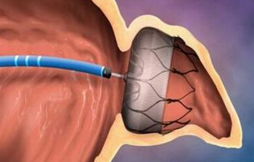
ESC-EHRA心房颤动消融长期注册是一项前瞻性的多国研究,旨在提供当代世界心房颤动(AFIB)消融的结果。近期,一项发表在Eur Heart J杂志上的文章评估了AFIB术后患者的生活现状。研究选取了27个欧洲国家共104个中心,登记20-50个患者首次进行并在此进行AFib消融。在网络电子病例记录表上记录了试验前、试验中及随后1年的随访数据。最后共有3630例患者,其中3593例接受AFib消
ESC-EHRA心房颤动消融长期注册是一项前瞻性的多国研究,旨在提供当代世界心房颤动(AFIB)消融的结果。
近期,一项发表在Eur Heart J杂志上的文章评估了AFIB术后患者的生活现状。
研究选取了27个欧洲国家共104个中心,登记20-50个患者首次进行并在此进行AFib消融。在网络电子病例记录表上记录了试验前、试验中及随后1年的随访数据。
最后共有3630例患者,其中3593例接受AFib消融(98.9%)。中位年龄为59岁,32.4%的患者有孤立性房颤。其中98.8%的患者尝试肺静脉隔离,成功率达到95-97%。
97%的受试者存在AFib相关症状。住院合并并发症的发生率为7.8%,一名患者因食管胃瘘死亡。
在3180(88.6%)名患者中进行为期一年的随访,消融后的中位时间为12.4个月(11.9-13.4):52.8%通过临床随访,44.2%通过电话联系,3.0%通过全科医生会诊。
在12个月内,有或没有抗心律失常药物(AAD)的成功患者占73.6%。大部分患者(46%)仍使用AAD上。晚期并发症包括14例死亡(4例心脏,4例血管,6例其他原因)和333例(10.7%)其他并发症。
此项调查表明:AFIB消融患者在临床中大多存在临床症状,目前总体成功率令人满意,但其并发症的发生率仍然较高,并且很大一部分患者仍然使用AAD上。消融后的监测差异仍然很大。消融后的抗血栓治疗指南仍然不足。
原始出处:
Arbelo E, Brugada J, Lundqvist CB, et al. Contemporary management of patients undergoing atrial fibrillation ablation: in-hospital and 1-year follow-up findings from the ESC-EHRA atrial fibrillation ablation long-term registry. Eur Heart J. 2017 Jan 18. pii: ehw564. doi: 10.1093/eurheartj/ehw564.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#并发#
35
#房颤消融术#
44
#房颤消融#
32
AFIB消融患者在临床中大多存在临床症状,目前总体成功率令人满意,但其并发症的发生率仍然较高,并且很大一部分患者仍然使用AAD上。消融后的监测差异仍然很大。消融后的抗血栓治疗指南仍然不足。
58
很好,不错,以后会多学习
63
#ART#
38
#消融#
34
#消融术#
36
#HEART#
31
#消融术#
34