Leukemia Res:阿那格雷在真性红细胞增多症中用于血小板定向细胞减少:从大型多中心数据库中洞察实用性和安全性结果
2022-09-11 将军的九分裤 MedSci原创
阿那格雷 (ANA) 是一种血小板特异性细胞减少剂,多用于高危原发性血小板增多症的指南指导管理。尽管耐受性有限,ANA仍是 PV 患者选择性血小板控制的有效选择
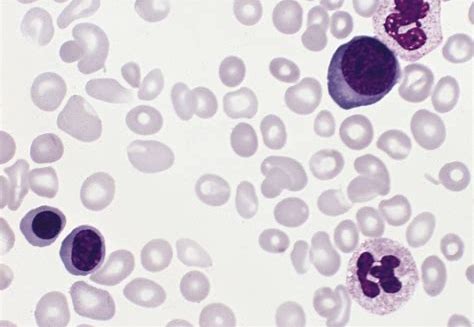
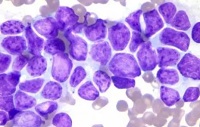
阿那格雷 (ANA) 是一种血小板特异性细胞减少剂,多用于高危原发性血小板增多症的指南指导管理。在真性红细胞增多症 (PV) 的背景下,ANA 偶尔用于临床实践,虽然不是指南指导的 PV 治疗的一部分,但 ANA 经常在临床实践中用作血小板降低剂,用于治疗伴有血小板增多症的 PV 患者。然而,这种方法的安全性和有效性尚未得到正式研究。此次报道的研究的目的是利用一个完善的、大型、多中心的 PV 患者数据库来回顾性描述接受 ANA 治疗的患者的特征和结果。
研究利用了来自美国 10 家机构的 527 名PV患者的既定数据库。对于初始数据库纳入,患者必须已被诊断为 2016 年世界卫生组织 (WHO) 标准所定义的 PV,并且已年满 18 岁。在 527 名 PV 患者的多中心队列中,48 名接受了 ANA(9 名因缺乏数据而被排除)。27 人 (69.2%) 有高危 PV,10 人 (25.6%) 曾有血栓形成,没有人有严重的血小板增多症、获得性血管性血友病和/或对羟基脲的耐药性。
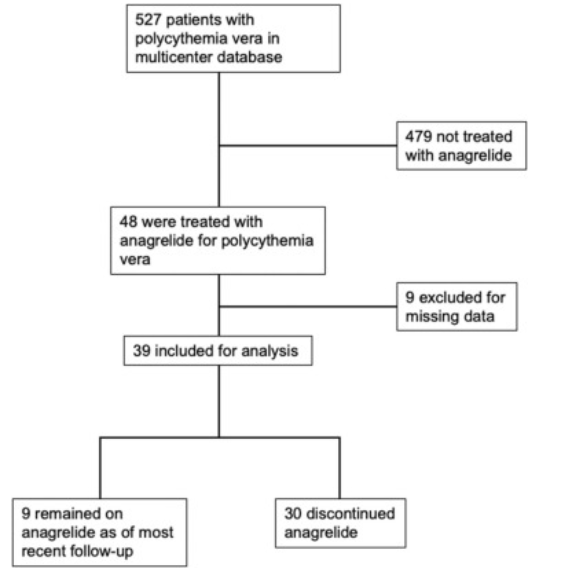
图1:流程图

图 2:阿那格雷停药时间的 Kaplan-Meier 曲线。
虽然 ANA 有效地降低了中位血小板计数,但 43。5% 的患者在 ANA 停药时有未解决的血小板增多症。治疗中出现的不良事件——包括头痛、心悸和心律失常、恶心、呕吐和/或腹泻——导致 76.9% 的患者停用 ANA。此外,三名患者在 ANA 治疗的中位持续时间为 27.5 个月期间经历了动脉血栓形成。
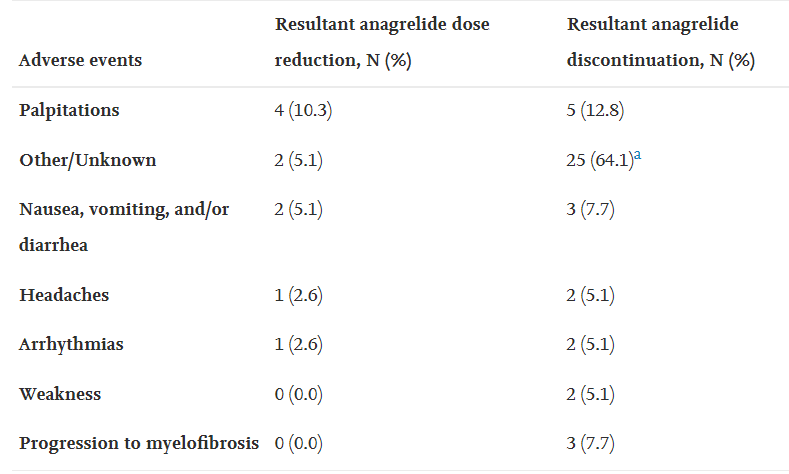
表:导致ANA剂量减少或停用的诱发事件。
总体而言,目前的研究表明,尽管耐受性有限,ANA仍是 PV 患者选择性血小板控制的有效选择。在接受 ANA 治疗的 PV 患者队列中,血栓并发症(7.7%)和因毒性而停止治疗的发生率(76.9%)值得注意。目前的数据表明,将血小板目标作为 PV 的治疗终点缺乏明确的益处,相反,PV患者可以通过持续使用低剂量阿司匹林来降低血栓风险,从而靶使PV相关的血栓烷生物合成增加。在评估 ANA 在 PV 中的作用的大型前瞻性研究之前,研究人员建议考虑到伴有出血风险和症状性血小板增多症的 PV 患者,可使用血小板定向细胞减灭术。即使在这些情况下,他们也提倡使用非选择性细胞减灭剂,例如 HU 和 IFN-α。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#多中心#
51
#实用性#
42
#定向#
41
#红细胞#
40
#红细胞增多症#
41