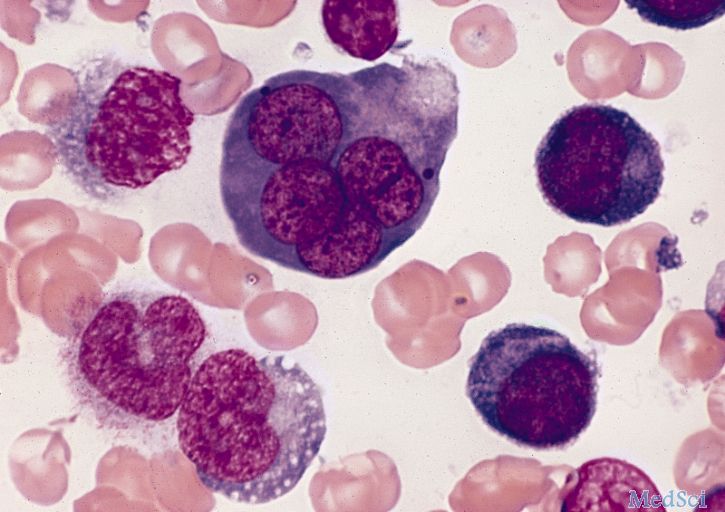
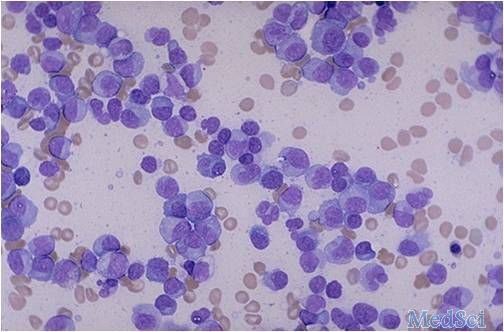
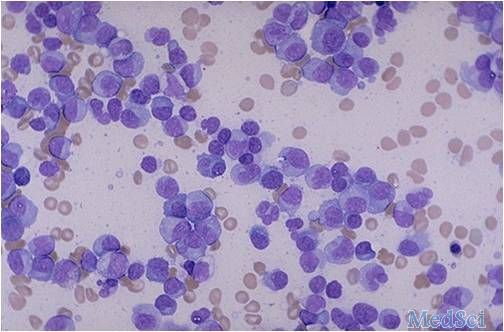
Blood:移植物产生的AML特异性抗体可特异性杀伤白血病原始细胞。
2017-10-25 qinqiyun MedSci原创
大部分急性髓系白血病(AML)患者仅能通过同种异体造血干细胞移植(HSCT)诱导移植物抵抗白血病免疫反应(GvL)来治愈。虽然T细胞和NK细胞在肿瘤免疫过程中的作用已熟为人知,但对B细胞在该过程中的作用知之甚少。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#特异性#
31
#植物#
46
#特异性抗体#
29
#移植物#
28
学习了一个人
76