Blood:在VHL基因内含子中发现神秘外显子,突变可导致红细胞增多症或VHL病
2018-06-13 MedSci MedSci原创
中心点:在家族性红细胞增多症或von Hippel-Lindau病患者中发现VHL神秘外显子突变。VHL基因2号外显子上的同义突变或可导致外显子跳跃,从而引发家族性红细胞增多症或或von Hippel-Lindau病。摘要:Chuvash红细胞增多症是一种常染色体隐形遗传的红细胞增多症,与von Hippel-Lindau(VHL)基因上的纯合p.Arg200Trp突变相关。自发现上述致病突变后,
在家族性红细胞增多症或von Hippel-Lindau病患者中发现VHL神秘外显子突变。
VHL基因2号外显子上的同义突变或可导致外显子跳跃,从而引发家族性红细胞增多症或或von Hippel-Lindau病。
摘要:
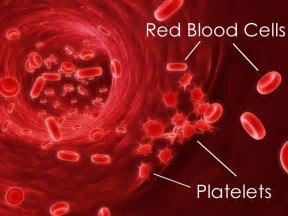
Chuvash红细胞增多症是一种常染色体隐形遗传的红细胞增多症,与von Hippel-Lindau(VHL)基因上的纯合p.Arg200Trp突变相关。自发现上述致病突变后,在先天性红细胞增多症患者中陆续发现更多的纯合或杂合的VHL突变。VHL是一种重要的肿瘤抑制基因,其突变最早是在von Hippel-Lindau病(高度血管化肿瘤)患者中发现的。
Marion Lenglet等人近期在VHL的1号内含子深处发现一新的神秘外显子(命名E1’),E1’在多种组织中自然表达。而且,研究人员在七个红细胞增多症家系中发现E1'突变(1例纯合、6例复合杂合突变[1个E1'突变+1个VHL编码区突变]);另外在一个典型VHL病的大家系中也发现E1'突变,而且在VHL的其他外显子上无任何变异。
研究人员发现突变导致VHL剪接失调、E1'过度保留,进而导致VHL蛋白表达减少。此外,研究人员在五个红细胞增多症或VHL疾病的家系中发现VHL2号外显子上的同义突变具有致病作用,可通过E2跳跃改变剪接。
在本研究囊括的所有病例中,突变差异性影响剪接,与表型严重程度相关。本研究证实神秘外显子保留或外显子跳跃是VHL新的改变方式,揭示了VHL基因的复杂剪接调控。本研究结果为VHL相关的缺氧信号通路的诊断和研究开辟了新的途径。
原始出处:
Marion Lenglet,et al.New lessons from an old gene: complex splicing and a novel cryptic exon in VHL gene cause erythrocytosis and VHL disease. Blood 2018 :blood-2018-03-838235; doi: https://doi.org/10.1182/blood-2018-03-838235
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#VHL#
39
#红细胞#
32
#红细胞增多症#
47
#外显子#
34
学习谢谢分享
98
看看
66