NEJM:RESCUE-Japan LIMIT研究:大面积急性缺血性卒中患者血管内治疗的功能预后优于单纯药物治疗
2022-02-12 “ 心关注”公众号 “ 心关注”公众号
近日,发表在N Engl J Med杂志上的一项研究发现,与仅接受标准药物治疗的急性缺血性卒中患者相比,联合接受血管内治疗(机械取栓)的患者其功能预后更佳,但颅内出血较多。
近日,发表在N Engl J Med杂志上的一项研究发现,与仅接受标准药物治疗的急性缺血性卒中患者相比,联合接受血管内治疗(机械取栓)的患者其功能预后更佳,但颅内出血较多。
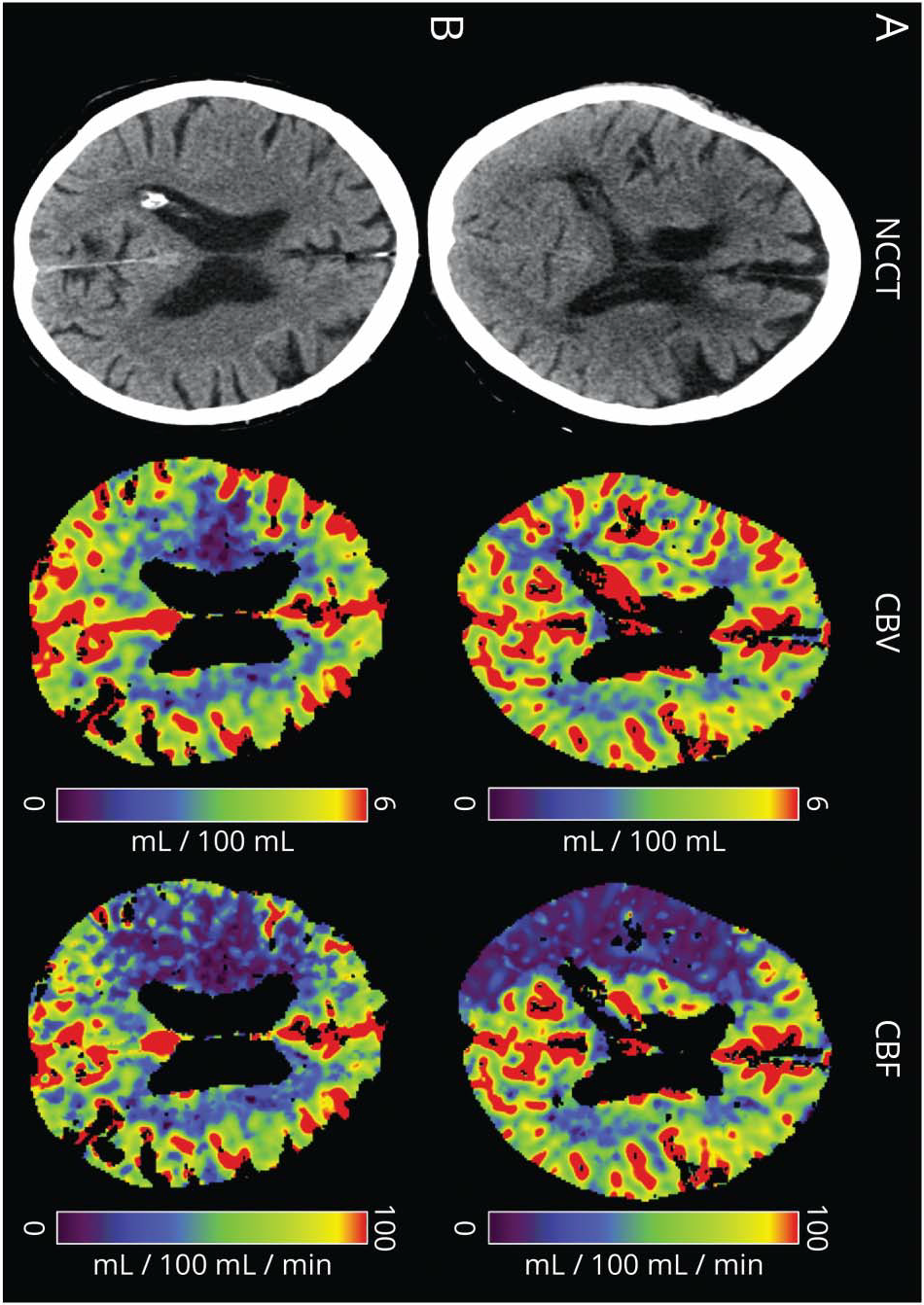
血管内治疗已经成为急性脑卒中标准化治疗的方法之一。指南建议,当大脑中动脉M1段或颈内动脉闭塞、影像学提示梗死区域(也称为缺血核心)不大、阿尔伯塔卒中项目早期CT评分(ASPECTS)至少为6(范围从0到10,值越低表明梗死区域越大)或缺血核心容积与延迟灌注区容积不匹配时,应考虑血管内治疗。
考虑到再灌注后梗死区域的出血风险,梗死面积较大的患者(ASPECTS评分≤5)通常被排除在血管内治疗的临床试验之外。一项对观察性研究的荟萃分析表明,在ASPECTS评分≤5的患者中,与单独治疗相比,血管内治疗可能具有更好的功能预后和更低的90天死亡率。为明确其中联系,研究人员在日本开展了一项多中心、开放标签、随机临床试验,纳入ASPECTS评分为3~5的急性脑卒中患者。所有纳入患者以1:1的比例随机分配至血管内治疗组(机械取栓+常规医疗护理)和常规医疗护理组。主要结果是90天时0~3的改良Rankin量表评分(评分范围为0至6分,分数越高表示残疾越严重);次要结果包括90天时改良的Rankin量表评分的好转范围及入院48小时的NIHSS评分至少提高8分的比率。
研究结果
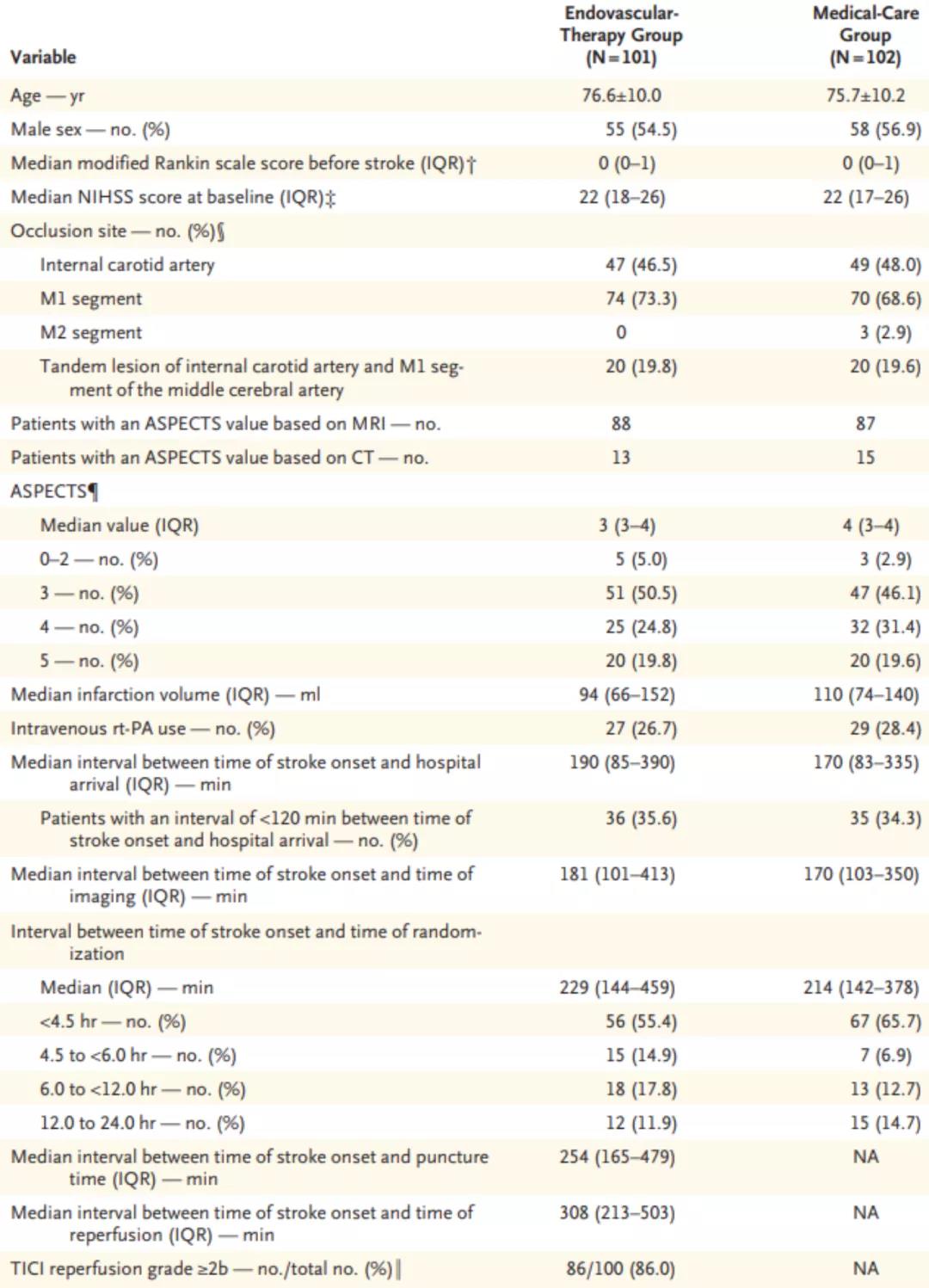
从2018年11月到2021年9月,共有203例患者入组;101人被分配到血管内治疗组,102 人被分配到常规医疗护理组;最终有202例患者于2021年12月完成随访并被纳入主要分析。基线时两组患者的人口统计学特征和临床特征相似(表1),平均年龄76岁,44.3%为女性。入院时NIHSS评分中位数为22,ASPECTS评分中位数为3。47.3%的患者发生颈内动脉闭塞,70.9%的患者发生大脑中动脉M1段闭塞。59%的患者出现心房颤动,每组约27%的患者接受了人类重组组织型纤溶酶原激活物(rt-PA)治疗。86.0%的血管内治疗组患者的TICI再灌注等级为2b或更高。
表1. 患者基线临床和影像学特征
血管内治疗组和常规医疗护理组90天时改良Rankin量表评分为0至3分的患者百分比分别为31.0%和12.7%(RR 2.43,95%CI 1.35-4.37;P=0.002)(表2)。血管内治疗组的改良Rankin量表评分的好转范围优于常规医疗护理组(OR 2.42,95%CI 1.46-4.01)(图1)。血管内治疗组和常规医疗护理组入院后48小时NIHSS改善至少8分的患者百分比分别为31.0%和8.8%(RR 3.51.95%CI 1.76-7.00)。
表2. 临床结局
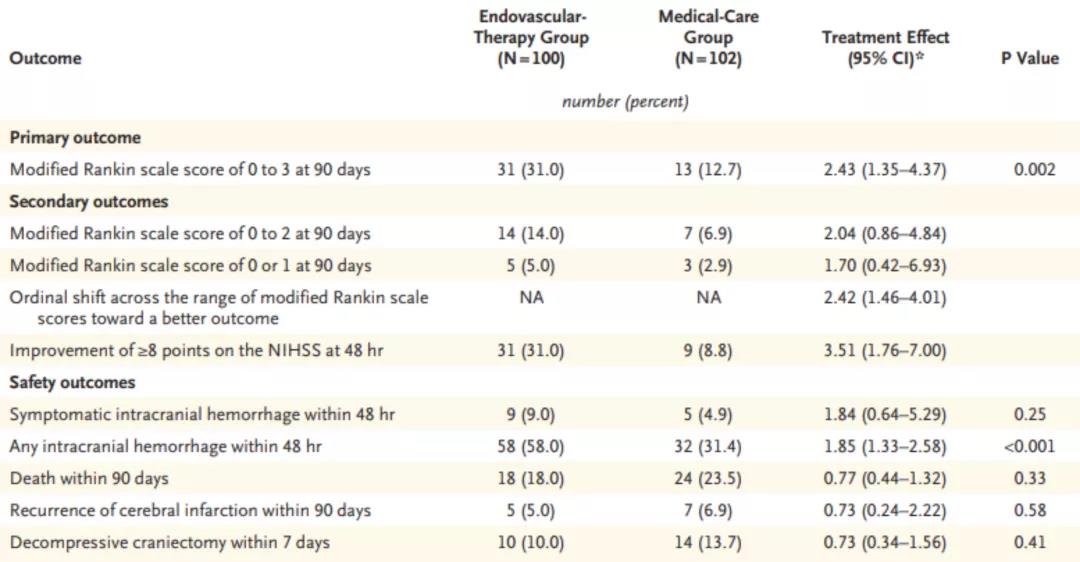
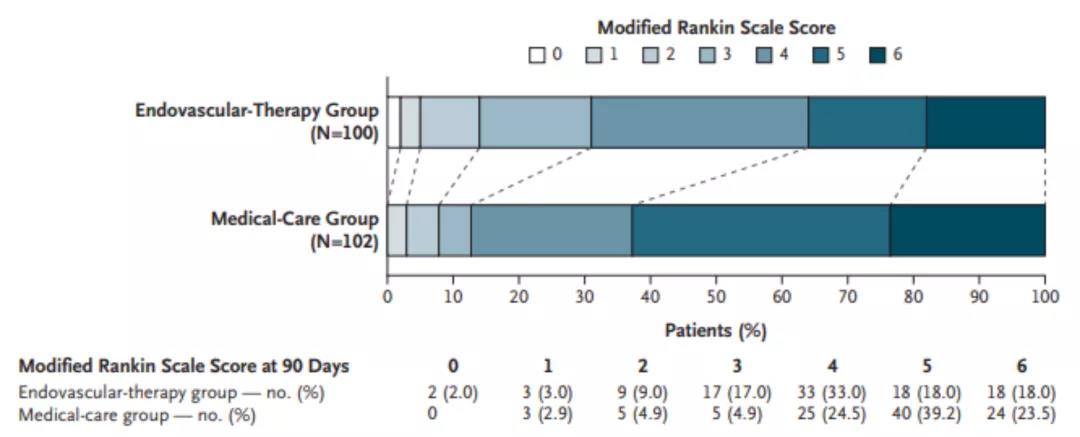
图1. 90 天时改良Rankin量表分数的分布
血管内治疗组48小时内任何颅内出血的发生率高于常规医疗护理组(58.0% vs. 31.4%;RR 1.85,95%CI 1.33-2.58;P<0.001),但48小时内有症状的颅内出血或90天时的死亡没有显着组间差异(表2)。33.7%的血管内治疗组患者和18.6%的常规医疗护理组患者发生了其他不良事件,其中心血管事件分别为9.9%和2.9%。
原始出处:
Yoshimura S, Sakai N, Yamagami H, et al. Endovascular Therapy for Acute Stroke with a Large Ischemic Region. N Engl J Med. 2022 Feb 9. doi: 10.1056/NEJMoa2118191. Epub ahead of print. PMID: 35138767.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#MIT#
51
#缺血性卒#
33
#缺血性卒中患者#
35
#大面积#
43
#缺血性#
36
#卒中患者#
25
#APA#
37
#功能预后#
38
血管内治疗需要介入,如果能静脉在基层应用前景更广
43