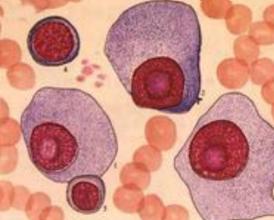
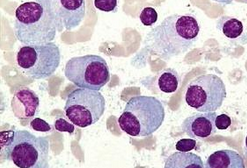
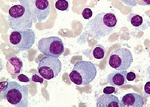
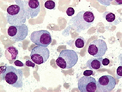
NEJM:Daratumumab+来那度胺+地塞米松治疗多发性骨髓瘤疗效显著
2016-10-06 MedSci MedSci原创
在一项涉及复发或难治性多发性骨髓瘤患者的1-2阶段研究中,Daratumumab单独治疗,与来那度胺和地塞米松联合治疗都显示出了较好的功效。原始出处:Meletios A. Dimopoulos,Albert Oriol,Hareth Nahi,et al.Daratumumab, Lenalidomide, and Dexamethasone for Multiple Myeloma,NEJM,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#多发性#
28
#mAb#
30
学习了,继续关注
67
好文章,受益
64
文章很好,继续关注
61
#Daratumumab#
27