重磅:CAR-T首次消灭实体瘤,意义非凡!
2016-12-29 应雨妍 奇点网
一大早打开电脑,就迎面被一个大新闻“撞了一下腰”——CAR-T疗法首次在实体瘤治疗中获得了突破!奇点糕一下就心潮澎湃了有没有!这个被CAR-T“盯上”的实体瘤还恰好是非常“难缠的”胶质母细胞瘤。这么厉害的研究在今天发表在了临床领域顶级期刊《新英格兰医学杂志》上[1]。这项研究是由希望之城(City of Hope)研究中心做的,希望之城位于美国加州,是一所顶尖的非盈利研究治疗中心,也是美国国家
一大早打开电脑,就迎面被一个大新闻“撞了一下腰”——CAR-T疗法首次在实体瘤治疗中获得了突破!奇点糕一下就心潮澎湃了有没有!这个被CAR-T“盯上”的实体瘤还恰好是非常“难缠的”胶质母细胞瘤。
这么厉害的研究在今天发表在了临床领域顶级期刊《新英格兰医学杂志》上[1]。这项研究是由希望之城(City of Hope)研究中心做的,希望之城位于美国加州,是一所顶尖的非盈利研究治疗中心,也是美国国家癌症研究中心认证的47所综合癌症研究中心之一。

希望之城研究中心
接受治疗的是一名50岁的男性患者,他患的是复发性多灶胶质母细胞瘤,在接受了肿瘤切除、化疗还有放疗之后,肿瘤依然没有离他而去,于是“走投无路”的他加入了希望之城的I期临床研究中(临床注册号:NCT02208362)。研究人员通过磁共振成像(MRI)确定了患者脑内共有5个肿瘤灶,最大的一个位于右颞枕区域(tumor 1,简称t1,后同),剩下的两个位于右额叶(t2、t3),两个位于左颞叶(t4、t5)。其中t2、t3在之前接受过不完全切除,在这次的治疗开始后,它们的附近又出现了两个肿瘤(t6、t7)。

接受治疗的患者Richard Grady
研究人员靶定的抗原是IL13Rα2,这是脑瘤中的一种常见受体,但同时这个靶点是首次在CAR-T研究中出现。他们采用的是脑室内注射的方法,注射点位于t1附近,第一次的治疗持续了6周时间,但是情况并不乐观,t1虽然没有变大,但是仍然顽固地占据着位置,而t4-t7四个肿瘤灶都有了小幅的增长。更糟糕的是,患者出现了腿麻的症状,经MRI检查,研究人员发现了脊柱转移,出现了一个18mm的大肿瘤和几个不到4mm的小肿瘤!这让研究人员有些担心,他们做了分析,认为CAR-T治疗是起到了阻止肿瘤生长的作用的,但是只局限在了局部(t1注射点),对较远位置的肿瘤没有起到有效的控制。

Richard接受脑室内注射
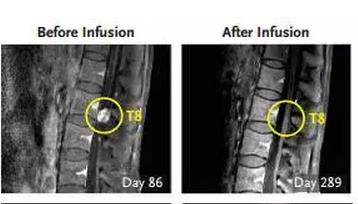
在此基础上,第二次治疗开始了,研究人员在右侧脑室进行了10次注射。注射进行了3次(实验的第133天)后,研究人员被一个喜讯“唤醒”——患者脑内和脊柱内的所有肿瘤都变小了!紧接着,在第5次注射(第190天)后,部分肿瘤消失了,剩下一部分减小了77%。在剩下的5次注射结束后,研究人员发现,患者体内的肿瘤全都消失了!
CAR-T消灭肿瘤细胞的过程
经过MRI和PET(正电子发射断层扫描,灵敏度和特异性更高,可在病变区的形态结构尚未呈现异常时就发现,还可鉴别肿瘤良恶性,并且可以全身成像)检查,都没有发现有肿瘤的迹象。而且患者在治疗中几乎没有出现什么严重的副作用,这一点也很重要,要知道,就是因为CAR-T疗法严重的神经毒性,导致JUNO公司CAR-T的II期临床试验中2名患者死亡,试验也曾短暂地被FDA叫停。
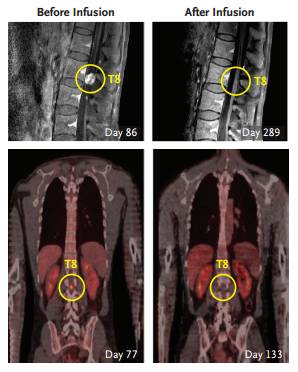
患者脊柱位置转移瘤在不同治疗时间的成像示意图
研究的通讯作者,希望之城的神经外科主任,Behnam Badie博士告诉STAT news,这个结果真的是“充满了戏剧性”,他的父亲10年前因为胶质母细胞瘤去世了,他没有想到,用CAR-T治疗胶质母细胞而且取得阶段性成功的这一天会来的这么快[2]。不过不太幸运的是,当试验往前推进,到了7.5个月(228天)的时候,研究人员在4个新的位置发现了复发。

Behnam Badie博士
唯一令人感到安慰的是,新肿瘤的出现与前7个肿瘤灶不但不相邻,甚至可以说是相隔甚远,这说明CAR-T疗法所产生的抗体还是起到了作用的,回想起前面第一次治疗效果的不理想,这个结果或许是“有迹可循”的。对于准确的复发原因,研究人员还在调查之中,不过初步的结果已经显示,IL13Rα2的表达量减少了。
虽然,这是一个不完美的研究,但是就像研究的第一作者,Christine Brown博士说的那样“我们的研究最令人兴奋是,它证明了一个更好的治疗方法是可能实现的。我们这个病人,他的肿瘤是‘具有侵略性的’、易转移的多灶型胶质母细胞瘤,而我们看到了所有病灶的消失,包括脊柱内的,迄今为止,这是第一次。”

Christine Brown博士
对于这个“既是成功也是失败”的结果,当然不会缺少怀疑的声音,来自俄勒冈健康与科学大学(the Oregon Health and Sciences University)的血液肿瘤学家Vinay Prasad博士认为这可能只是“昙花一现”,他通过邮件提出了一连串的质疑:“仅仅一个患者成功了,那其他的患者呢?CAR-T疗法会比其他疗法更好吗?接受CAR-T治疗的患者是会活得更久还是活得更好呢?这些都是未知数,研究人员不应该太乐观了。”
对此,纪念斯隆-凯特林癌症中心的专门从事CAR-T治疗的Jae Park博士认为,“目前我们还不能说它解决了实体瘤的问题,但它确实首次向我们证明了CAR-T治疗胶质母细胞瘤的效果,也让我们知道了CAR-T也许是能突破实体瘤这个‘底线’的。”奇点糕也认为,这是一次很有意义的尝试,虽然它还处于一个初级阶段,虽然可能是条弯路,但这也是一条“充满了希望”的弯路。
原始出处:
Christine E. Brown, Ph.D., Darya Alizadeh, Ph.D., et all. Regression of Glioblastoma after Chimeric Antigen Receptor T-Cell Therapy. N Engl J Med 2016; 375:2561-2569
https://www.statnews.com/2016/12/28/car-t-brain-cancer/
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#CAR-#
23
很好,不错,以后会多学习
64
#重磅#
24
继续前进吧,实验就是需要挑战一些多数人认为不可能的东西!
60
代价大吗?如果只是局部消失,那放疗完全可以做到,立体定向放疗甚至更好
61
不值得羡慕
0
不错的实验。
66
cool
27
学习了!!!!!!!
27
有意义的研究
27