BMJ子刊:注意!一线医护人员多睡1小时,感染COVID-19的风险降低12%!
2021-04-03 MedSci原创 MedSci原创
最新的研究发现,新冠抗疫期间,长期高压高风险的工作状态导致的失眠、倦怠,会反之进一步增加医护人员受感染的风险。因此,有必要采取措施,更合理地评估医护人员工作压力,优化轮休制度,保证职业安全。
全球新冠疫情大流行期间,前线医护人员在抗击疫情中发挥着重要作用。有研究显示,相比于普通医护人员来说,奋斗在一线的医护人员感染COVID-19风险高出1.8倍至3.3倍。而同时我们也认识到,睡眠障碍,职业倦怠等造成的身体慢性疲劳可增加传染病的感染风险。而这些因素是否也会增加COVID-19感染风险,目前还没有研究明确。
近期,发表在BMJ Nutrition Prevention & Health上的一项研究表明,失眠、睡眠中断和日常倦怠不仅增加医护人员COVID-19感染风险,还可加重COVID-19感染,并导致更长的恢复期。
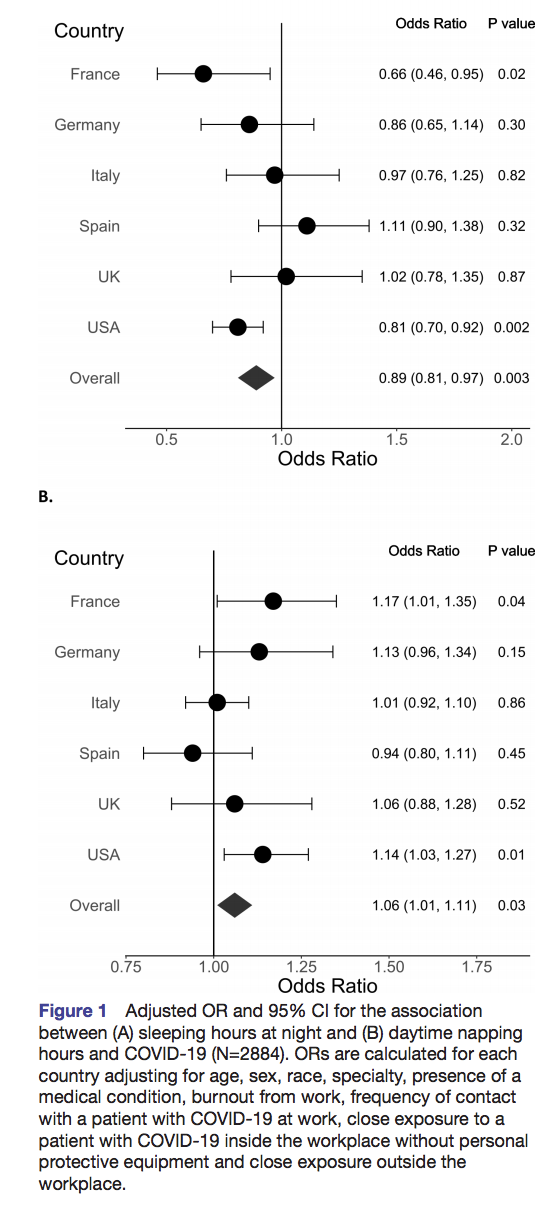
在这项研究中,研究人员对来自2020年7月17日至2020年9月25日全球6个国家,法国、德国、意大利、西班牙、英国和美国的2884名医护人员进行调查,评估了睡眠和日常倦怠是否是感染COVID-19的高危因素。这些医护人员主要来自重症监护,急诊医学以及内科医学等领域,并反复暴露在COVID-19感染患者中。研究人员收集了所有医护人员的个人生活资料,包括生活方式、健康状况、药物使用和膳食补充剂的使用等详细资料,另外还收集在过去一年中夜间和白天小睡的睡眠时间;是否存在睡眠问题,工作倦怠以及工作场所接触COVID-19感染的情况。
研究结果显示,在所有纳入研究的医护人员中,有568名医护人员感染COVID-19。夜间睡眠时间平均在7小时以下,但超过6小时。约1/4的COVID-19感染者出现夜间入睡困难,而未感染者夜间入睡困难发生率大约为1/5。

另外,调整混杂因素后统计分析,夜间睡眠时间每增加1小时,感染COVID-19的几率就会降低12%。与那些没有睡眠问题的人相比,失眠、睡眠中断和日常倦怠的医护人员感染COVID-19的几率高88%。与那些没有任何倦怠的医护人员相比,那些每天都会出现倦怠的医护人员感染COVID-19的可能性要高出2倍,而且感染者情况更加严重,需要更长的恢复期。
综上,夜间睡眠不足,严重的睡眠问题和高度的职业倦怠可能是一线医护人员感染COVID-19的高危风险因素。因此,如果出现职业倦怠,则需要高质量的睡眠和再充电时间,以防止倦怠及其后果。从职业和生活方式医学的角度来看,更好地了解轮班工作和睡眠的影响对于医护人员和至关重要。
原始出处
Hyunju Kim1,2, Sheila Hegde3,4, Christine LaFiura5, Madhunika Raghavan5, Eric Luong6, Susan Cheng6, Casey M Rebholz1,2 and Sara B Seidelmann7,8.COVID-19 illness in relation to sleep and burnout, BMJ Nutrition Prevention & Health, DOI: 10.1136/bmjnph-2021-000228
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#风险降低#
23
#BMJ#
22
#医护人员#
26