Gastroenterology:溃疡性结肠炎相关结直肠癌监测该用随机活检还是针对性活检?
2016-08-29 Moon 译 MedSci原创
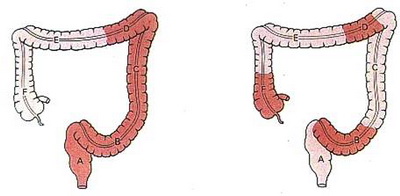
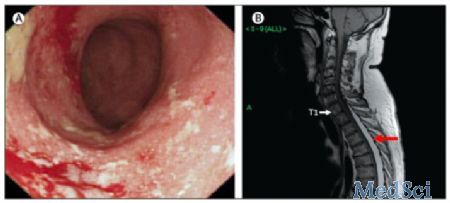
随机活检被推荐用于溃疡性结肠炎(UC)相关的结直肠癌的监测。然而,有针对性的活检可能是更有效的。我们进行了一项随机对照试验,对UC患者针对性的或随机活检的瘤样检出率进行了比较。 研究纳入了246名UC病程≥7年的患者,来自日本的52个机构(2008年10月1日至2010年12月31日)。患者被随机分配到随机组(除了有针对性的活组织切片检查外,每10厘米收集活检标本, n=122)或针对目标组
随机活检被推荐用于溃疡性结肠炎(UC)相关的结直肠癌的监测。然而,有针对性的活检可能是更有效的。我们进行了一项随机对照试验,对UC患者针对性的或随机活检的瘤样检出率进行了比较。
研究纳入了246名UC病程≥7年的患者,来自日本的52个机构(2008年10月1日至2010年12月31日)。患者被随机分配到随机组(除了有针对性的活组织切片检查外,每10厘米收集活检标本, n=122)或针对目标组(从可疑瘤位置收集活组织切片检查,n=124)。主要终点是单一结肠镜检查中发现的肿瘤性病变的数量。对组间肿瘤性病变平均数的比例和差异进行评估。我们还进行了组间非劣效性评估作为探索性的研究;肿瘤性病变平均数的比率非劣性的边缘值为0.65 (=0.13/0.20)。
每结肠镜检查发现含有肿瘤组织的活组织切片检查平均数在目标组和随机组分别为0.211 (24/114)和0.168 (18/107)(比例为 1.251; 95% CI = 0.679 to 2.306)。下限值高于非劣性边缘值0.65。目标组和随机组患者中分别有11.4%和9.3%的患者检出肿瘤(P=.617)。随机组的活检样本数量更多(34.8 vs 3.1 , P<.001),总检查时间更长(41.7 vs 26.6分钟, P<.001)。在随机组中,随机活检发现肿瘤组织的标本来自于既往或现在存在炎症的区域。
随机对照试验结果表明,针对性和随机活检检测肿瘤的比例相似。然而,有针对性的活检似乎是一个更具成本效益的方法。
原始出处:
Watanabe T.et al. Comparison of Targeted vs Random Biopsies for Surveillance of Ulcerative Colitis-associated Colorectal Cancer. Gastroenterology. 2016 August 11.

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#GAS#
39
#结肠炎相关#
40
#AST#
28
文章很好值得关注
56
文章不错,继续学习
63
#溃疡性#
26
努力学习。。。
63
内容很好的
53
同意针对性活检。
79
很好,不错,以后会多学习
27