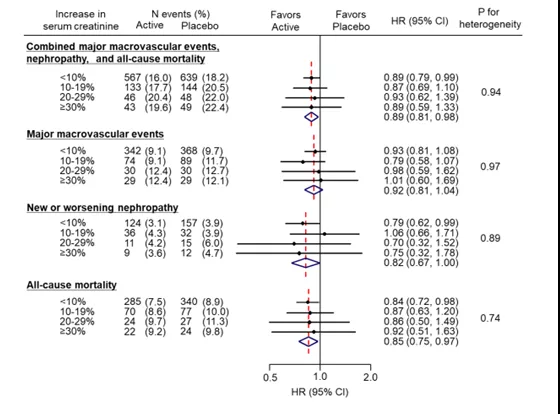
ADVANCE研究全新分析:糖尿病患者应用ACEI短期肌酐增加≥30%或不应停药?
2019-09-20 佚名 中国循环杂志
高血压和蛋白尿是肾脏病进展的独立危险因素,而血管紧张素转换酶抑制剂(ACEI)类药物可通过作用于肾素-血管紧张素-醛固酮系统(RAAS)来改善肾脏血流动力学,有效降低尿蛋白,改善高血压预后,比如多项研究显示,培哚普利有助于显着改善慢性肾病患者蛋白尿,降低慢性肾病患者肾功能衰竭发生率[1-2]。鉴于ACEI全面的心肾保护作用,不论是中国糖尿病肾病防治指南[3],还是新近欧洲心脏病学会(ESC)发
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#ACE#
38
#肌酐#
43
#停药#
28
#糖尿病患者#
40
学习了,学习了
69
谢谢MedSci提供最新的资讯
39