Hypertension:MitoQ,靶向线粒体的抗氧化剂,有望治疗老化的血管功能障碍
2018-04-17 MedSci MedSci原创
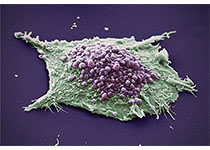
线粒体产生的活性氧过量是年龄相关的血管功能障碍的关键机制。Matthew J. Rossman等人实验室已证实予以线粒体为靶点的抗氧化剂MitoQ可通过减少线粒体产生的活性氧,从而改善血管内皮细胞功能,同时还可减轻年老小鼠的动脉僵硬,但在用于人类的效果不明。现Matthew J. Rossman等人产生将其预临床发现应用于人类,以明确MitoQ的安全性和疗效。开展一安慰剂为对照的双盲交叉设计研究,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#PE#
31
#TENS#
0
#MIT#
34
#氧化剂#
33
#老化#
0
#功能障碍#
27
#抗氧化剂#
42
#Hypertension#
22
#血管功能#
30
学习了
56