Blood:达雷木单抗治疗AL淀粉样变的疗效和安全性
2020-02-01 QQY MedSci原创
中心点:达雷木单抗(Daratumumab)用于AL淀粉样变性患者的耐受性良好。达雷木单抗用于既往治疗过的AL淀粉样变患者,可促进获得快速深层次的血液学缓解。摘要:达雷木单抗,是一种单克隆CD38单抗,已获得批准用于治疗骨髓瘤,但其用于AL淀粉样变的疗效和安全性尚未完全明确。研究人员开展一项前瞻性的II期试验,研究达雷木单抗单药疗法用于治疗轻链淀粉样变(AL)的安全性、耐受性和血液学及临床反应。共
达雷木单抗(Daratumumab)用于AL淀粉样变性患者的耐受性良好。
达雷木单抗用于既往治疗过的AL淀粉样变患者,可促进获得快速深层次的血液学缓解。
摘要:
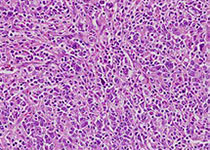
达雷木单抗,是一种单克隆CD38单抗,已获得批准用于治疗骨髓瘤,但其用于AL淀粉样变的疗效和安全性尚未完全明确。
予以所有患者达雷木单抗(16 mg/kg)治疗,静脉输注,1次/周,连续用8周,随后每2周一次,24周后,改为4周一次,直至病情进展或出现不可耐受的毒性,共24个月。
大多数患者接受了大剂量美法仑和干细胞移植以及/或蛋白酶体抑制剂治疗。既往治疗和招募进该试验的间隔中位时间为9个月。无3-4级输液相关反应发生。
86%的患者获得血液学完全和较好的部分缓解。首次和最佳血液学缓解的中位时间分别为4周和3个月。15位累及肾脏的患者中有10位(67%)获得肾脏缓解,14位累及心脏的患者中有7位(50%)获得心脏缓解。
总而言之,达雷木单抗用于复发性AL淀粉样变患者的耐受性良好,可使患者获得快速深层次的血液学缓解和器官缓解。
原始出处:
Vaishali Sanchorawala, et al.Safety, Tolerability, and Response Rates of Daratumumab in Relapsed AL Amyloidosis: Results of a Phase II Study.Blood. January 24, 2020.
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#疗效和安全性#
19
#淀粉样变#
25
#达雷木单抗#
36
#AL淀粉样变#
33
谢谢梅斯提供这么好的信息,学到很多
45