JCEM:先天性肾上腺增生骨折发生率的增加
2022-04-03 从医路漫漫 MedSci原创
CAH与发病率和死亡率增加有关,这种增加很大程度上可能与糖皮质激素替代过多或过少有关。
背景:先天性肾上腺增生(CAH)属于一组影响肾上腺皮质类固醇合成的常染色体隐性疾病,导致可变皮质醇,在大多数变体中还导致醛固酮缺乏,以及肾上腺雄激素过度产生。由CYP21A2基因突变引起的21-羟化酶缺乏症(21OHD)是CAH的主要变体,影响95%至99%的所有病例。从表型上看,CAH可分为经典型和非经典型,前者包括盐耗(SW)和单纯性男性化(SV )( NC )。如果在生命的最初几周内没有开始糖皮质激素替代,则SW表型与生命不相容,而SV表型传统上在新生儿期在女孩中发现,因为生殖器不明确,在男孩中发现,因为出生后快速生长和男性化。然而,现在许多国家已经引入了21OHD的新生儿筛查,几乎所有经典病例都是在新生儿期诊断的。NC表型具有20%至70%的残留酶活性,导致比经典型更少的症状和体征
糖皮质激素补充是CAH的主要治疗方法,于20世纪50年代引入,使CAH西南部的患者得以存活,并减少了肾上腺雄激素的产生。然而,平衡治疗以避免高雄激素血症和皮质醇增多症对临床医生和患者都是一个挑战。充分抑制下丘脑-垂体-肾上腺轴所需的糖皮质激素剂量大多是超生理剂量,导致负面的临床结果
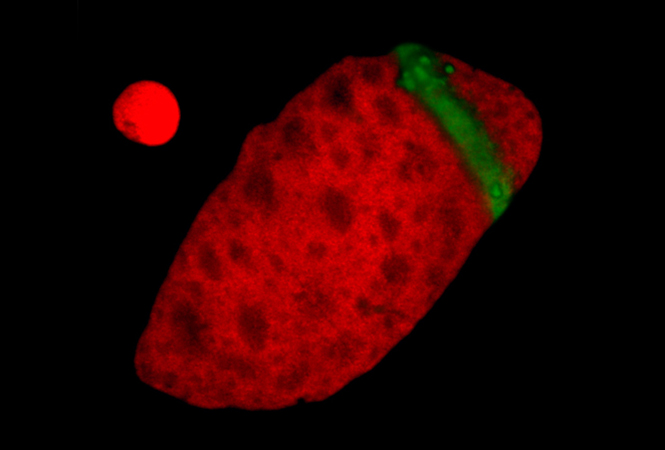
CAH与发病率和死亡率增加有关,这种增加很大程度上可能与糖皮质激素替代过多或过少有关。在接受免疫抑制剂量的患者中,糖皮质激素的使用与骨质疏松症之间存在明显的关联。糖皮质激素对骨骼有直接和间接的影响,导致最初的吸收增加和后来的骨形成减少,最终导致微结构变形和骨折风险增加。继发性甲状旁腺功能亢进也可能发生在使用糖皮质激素的患者中,因为糖皮质激素抑制肾小管中的钙重吸收。此外,性腺和肾上腺雄激素刺激两性的成骨细胞增殖和分化。已经证明硫酸脱氢表雄酮(DHEAS)和其他肾上腺雄激素影响骨代谢,主要是皮质骨,尤其是在肾上腺发育期间。患有典型CAH的儿童在儿童期缺乏DHEAS水平的生理上升,有效地解释了典型肾上腺皮质发育不全的原因。因此,由于肾上腺反应迟钝和糖皮质激素作用导致的低DHEAS水平会损害CAH患者的生长和成骨细胞功能,并可能是大多数患者骨密度(BMD)降低的原因;然而,并不是所有关于CAH患者骨密度的研究。在最近对患有CAH的成人进行的荟萃分析中,发现与匹配的对照组相比,BMD略有下降。此外,临床重要性不是BMD本身,而是脆性骨折,因为这些是骨质疏松症发病率的主要原因。然而,骨密度和骨折风险之间的联系,特别是在糖皮质激素诱导的骨质疏松症中,是很少的
目的:研究CAH骨折的患病率。
设计、地点和参与者:将CAH病患者(n = 714,全部21-羟化酶缺乏)与性别、出生年份和地点匹配的对照组(n = 71 400)进行比较。数据是通过连接各国基于人口的登记册获得的。
主要观察指标:骨折的数量和类型。
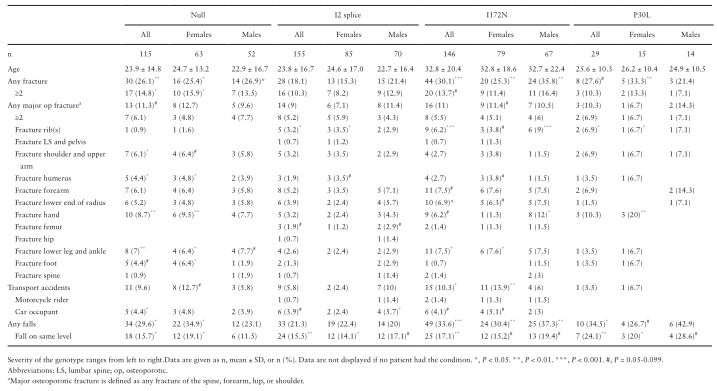
结果:平均年龄29.8±18.4岁。与对照组相比,CAH患者的骨折发生率更高[23.5%比16.1%,优势比(OR) 1.61,95%可信区间1.35-1.91],这种情况在男女两性中都有发现(女性:19.6%比13.3%,OR 1.57,95%可信区间1.23-2.02;男性:28.7%对19.6%,比值比为1.65,95%可信区间为1.29-2.12)。在引入新生儿筛查之前出生的患者骨折显著增加,而在之后出生的患者则没有。在所有CAH患者中,任何与骨质疏松症相关的主要骨折(脊柱、前臂、髋部或肩部)均增加(9.8%比7 .5%,OR 1.34,95% CI 1.05-1.72)。SV表型和I172N基因型的骨折患病率最高,而非经典表型和I2剪接基因型的骨折患病率没有增加。与对照组相比,无论男女,CAH病患者发生交通事故和在同一高度跌倒的几率更高。
表1 与年龄和性别匹配的对照组(每例100名对照组)相比,21-羟化酶缺乏所致先天性肾上腺增生患者的骨折率
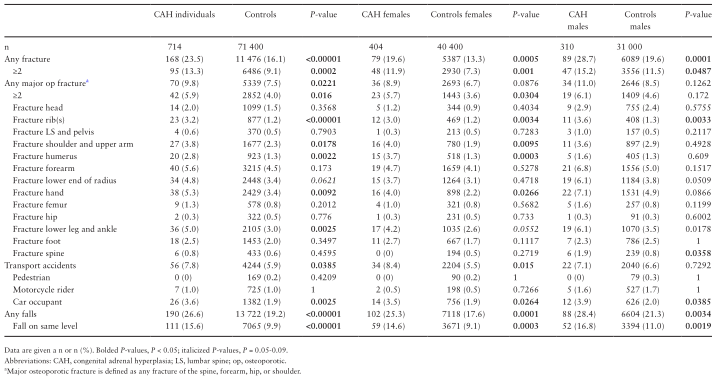
表2 21-羟化酶缺乏导致的先天性肾上腺增生患者的骨折分为不同的表型,并与年龄和性别匹配的对照组进行比较(每例100例对照)
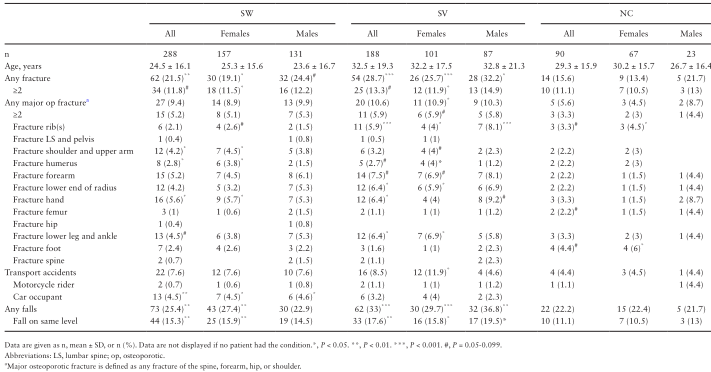
表3 与年龄和性别匹配的对照组(每例100例对照)相比,先天性肾上腺增生患者中的骨折构成四种最常见的CYP21A2基因型组
结论:CAH患者的任何骨折和与骨质疏松症相关的骨折的患病率均增加(包括男性和女性),但新生儿筛查的患者没有增加。我们的结论是,骨折风险评估和糖皮质激素优化应定期进行。
原文出处: Falhammar H, Frisén L, Hirschberg AL, et al.Increased Prevalence of Fractures in Congenital Adrenal Hyperplasia: A Swedish Population-based National Cohort Study.J Clin Endocrinol Metab 2022 01 18;107(2)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#发生率#
26
#肾上腺#
50
#JCEM#
33
#JCE#
23
#先天性肾上腺增生#
34
#先天性#
45