Am J Respir Crit Care Med:新的研究发现或可延长囊性纤维化患者的生存期
2016-05-14 MedSci MedSci原创
Am J Respir Crit Care Med:新的研究发现或可延长囊性纤维化患者的生存期近日,一项新的研究发现一种蛋白酶抑制剂(QUB-TL1)可阻断细胞中的离子通道从而显著减少气道炎症和感染的周期,研究人员表示,该分子或可延长肺囊肿性纤维化患者的生存期,该研究发现已在线发表于American Journal of Respiratory and Critical Care Medicine
该研究小组来自于英国贝尔法斯特女王大学,他们解释了QUB-TL1如何阻止上皮钠通道ENaC的激活。
实验中发现,该分子具有改善气道水合作用的潜能,且可显著改善粘液的清除。
该研究的通讯作者Lorraine Martin,来自女王大学药学院,说道:“这或可以预防感染和炎症慢性循环所造成的严重肺损伤,并可改善患者的生活质量以及预期寿命。”
囊性纤维化(CF)是一种遗传性疾病,可损害内脏器官,尤其是肺和消化系统。据WHO统计显示,全球约100000人患有CF。
随着治疗方法的不断提高,CF成年患者的数量也在稳定增加。仅30年前,CF患者还无法活到成年。而现在,约一半的CF患者可度过30岁,有的甚至可存活到50多岁和60多岁。
QUB-TL1抑制了一些通道激活酶
机体遗传了一个缺陷基因(CFTR)的两次错误拷贝从而可发生CF。均携带CFTR的夫妻孕育的后代发生CF的几率为25%。
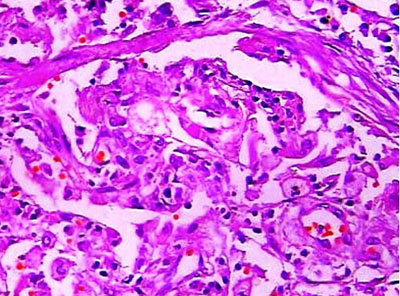
CFTR可破坏离子进出细胞的通道,从而导致粘液存留在组织表面上(如呼吸道和消化道内壁),使得组织表面脱水,变厚,便粘,且难以清除粘液。粘液可粘连细菌,引起慢性感染,炎症,肺部疤痕以及消化困难。
本研究中,研究人员测试了该分子在实验室培养的原代气道上皮细胞中的作用。结果发现,该分子可以抑制一些通道激活酶(包括前列腺蛋白,蛋白分解酵素,弗林蛋白酶),这些激活酶在CF气道上皮细胞表面活性异常高。抑制这些酶可降低钠通道的活性,从而改善机体的气道水合作用和粘液的清除。
作者认为,该研究发现或延缓或预防CFTR突变所致的CF患者肺部疾病的发展,从而延长患者的生存期。
原始出处:
James A Reihill et al., Inhibition of protease-ENaC signaling Improves mucociliary function in cystic fibrosis airways, American Journal of Respiratory and Critical Care Medicine, doi:10.1164/rccm.201511-2216OC, published online 25 March 2016.
Catharine Paddock. Cystic fibrosis: New molecule may prolong patient survival. MNT, 13 May 2016.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#囊性#
43
#研究发现#
32
#囊性纤维化患者#
20
不错哦继续关注
47
#生存期#
31
#Med#
0