Cancer Discov:科学家识别出与结直肠癌发生相关的特殊细菌蛋白
2022-01-31 转化医学 转化医学
与持续性细菌感染相关的慢性和低级别炎症或与结肠肿瘤的发生相关,然而,短暂性和自限性感染在细菌驱动的结肠肿瘤发生中的影响,研究人员尚不清楚。
与持续性细菌感染相关的慢性和低级别炎症或与结肠肿瘤的发生相关,然而,短暂性和自限性感染在细菌驱动的结肠肿瘤发生中的影响,研究人员尚不清楚。
近日,一篇发表在国际杂志Cancer Discovery上题为“Bacterial Genotoxin Accelerates Transient Infection–Driven Murine Colon Tumorigenesis”的研究报告中,来自约翰霍普金斯大学等机构的科学家们通过研究发现,引起常见食物中毒症状的细菌或许会产生一种损伤肠道细胞DNA的特殊毒素,从而潜在诱发结肠癌。这一研究发现或许提出了一种可能性,即全球每年大约200万例结肠癌病例中,有一些患者的发病或许是源于短暂且看似温和的食物中毒事件,同时研究者还指出了未来开发新型药物的可能性,即通过中和这种新发现的名为UshA的毒素来预防结直肠癌的发生。
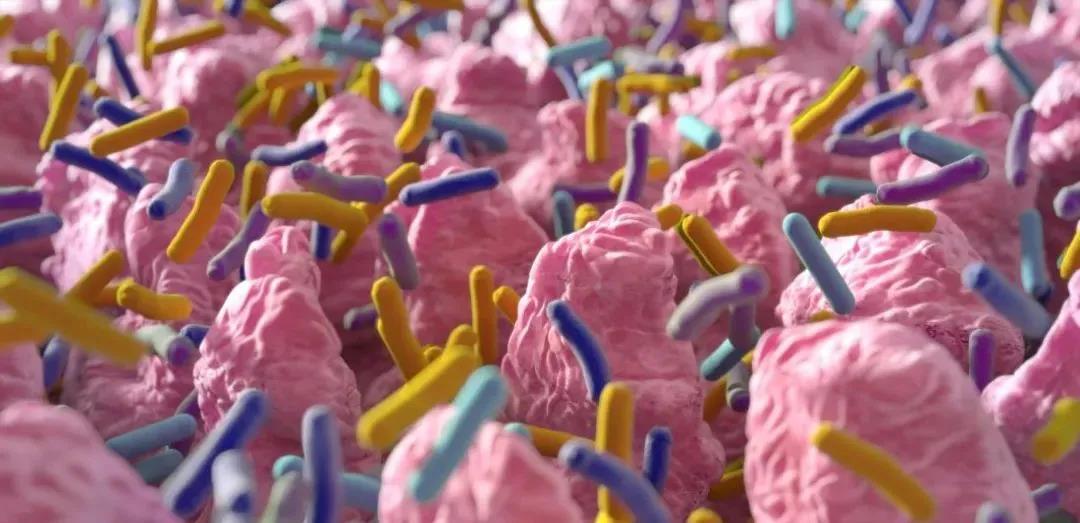
图片来源:Johns Hopkins University Bloomberg School of Public Health
此前研究结果表明,定植在肠道中的特定细菌或会通过参与慢性肠道炎症的持续性感染来诱发结直肠癌,引发食物中毒的短暂感染(包括旅行者腹泻,患者通常在1-2天内就能得到缓解)通常被认为是非致癌性的。研究者Fengyi Wan说道,我们希望本文研究或能促进其他科学家进行流行病学研究来调查短暂的腹泻感染和结肠癌发生之间的潜在关联。
这项研究中,研究人员利用柠檬酸杆菌来感染小鼠使其患上短暂性的腹泻疾病,这与人类感染上致泻大肠埃希氏菌的症状相似,结果发现,柠檬酸杆菌感染会迅速导致小鼠机体肠道内壁细胞出现明显的DNA损伤迹象。研究者注意到,这种损伤依赖于细菌中一种称之为III型分泌系统的机制,这种注射器样的附属物能被诸如柠檬酸杆菌和致泻大肠稀释菌用来向宿主细胞中注射蛋白质,这种机制有利于入侵的微生物生长和生存。
最终研究人员锁定了一种名为UshA的III型分泌系统注射蛋白,其或许是DNA损伤的原因,结果发现,致泻大肠埃希氏菌所产生的UshA蛋白或许含有一种具有分解DNA酶类活性的短片段;研究人员并不清楚DNA分解元件在柠檬酸杆菌生命周期中的功能,剔除该元件似乎会损伤细菌的生长或生存,但研究者在小鼠模型研究中发现证据表明,UshA或许会对被感染的宿主产生明确的致癌作用。
随后研究人员利用一种能自发形成结肠肿瘤的遗传工程化小鼠品系进行研究,结果发现,利用含有UshA的柠檬酸杆菌感染这些小鼠或许会明显加速其机体中肿瘤的形成;相比而言,感染了缺失UshA基因的工程化柠檬酸杆菌或许对于加速肿瘤的进展并没有任何影响。此外研究者还发现,柠檬酸加速的结肠肿瘤中的突变与人类结肠肿瘤中的突变类型高度相似,这或许再次强调了其与人类健康的潜在关联性。
图片来源:https://cancerdiscovery.aacrjournals.org/content/12/1/236#
这种关联性的有力确认或许并不容易实现,因为根据定义,短暂的感染在肿瘤发展时或许早已经消失了,在被检测出来之前,结肠肿瘤或许已经发展了很多年了;研究者Wan表示,建立携带UshA的微生物和人类结直肠癌之间的关联或许需要大量的流行病学研究,而且这些研究可能最好在撒哈拉以南的非洲地区进行,因为在这些地区,致泻性细菌感染和结直肠癌都非常常见。目前研究人员正在联合研究来开发针对UshA毒素的抑制剂,从原则上来讲,研究人员能给予已经存在腹泻疾病的患者这种抑制剂来保护其抵御促癌DNA损伤。
综上,本文研究结果表明,UshA或能作为细菌的III型分泌系统依赖性基因毒素,在促进的短暂和非侵袭性细菌感染加速结肠肿瘤发生过程中或许扮演着关键角色。
原始出处:
Yue Liu, Kai Fu, Eric M. Wier, et al. Bacterial Genotoxin Accelerates Transient Infection–Driven Murine Colon Tumorigenesis, Cancer Discovery (2022). DOI: 10.1158/2159-8290.CD-21-0912
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#细菌蛋白#
25
#Dis#
34
#结直肠#
23
#ISC#
34
学习了,谢谢分享
78