JCO:单抗Ramucirumab对转移性乳腺癌主要临床结局无益
2015-01-15 Jessie Li 译 MedSci原创
抗血管生成药用于肿瘤治疗是基于以下三点假设:①肿瘤的生长需要血管网络的不断扩张来供给营养和氧②可以通过治疗仅控制血管生成而对机体不产生其他毒副作用③这种疗法会使肿瘤休眠或增加化疗敏感性,从而发挥抗肿瘤作用 得益于VEGF家族中刺激血管生成因子和多个相关信号通路靶点的发现,研究者得以在临床检验上述三点假设。在结直肠癌、肾细胞癌、宫颈癌、卵巢上皮癌和非小细胞肺癌的治疗中抗血管生成药物的效果已得到
抗血管生成药用于肿瘤治疗是基于以下三点假设:
得益于VEGF家族中刺激血管生成因子和多个相关信号通路靶点的发现,研究者得以在临床检验上述三点假设。在结直肠癌、肾细胞癌、宫颈癌、卵巢上皮癌和非小细胞肺癌的治疗中抗血管生成药物的效果已得到肯定,但对转移性乳腺癌未见效。
Ramucirumab是VEGF2型受体抗体,是一种全人免疫球蛋白G1单克隆抗体,通过与VEGF2型受体的胞外区域结合,阻断VEGF与VEGF2型受体结合。而VEGF2型受体是血管生成、内皮增生、血管渗透性的主要调节因子,与乳腺癌转移及预后差有关。
随机对照试验已证实Ramucirumab能延长转移性胃癌和进展性非小细胞肺癌总生存期。但是,尚无研究检验其对乳腺癌的作用。2015年1月10日,JCO杂志刊登了Ramucirumab用于乳腺癌的三期临床试验(ROSE/TRIO-12)结果,其为一项双盲、安慰剂对照、随机、多国参与的研究。
2008年8月至2011年12月,纳入1144名HER2阴性的乳腺癌患者为研究对象,按2:1随机分为2组:多西他赛75mg/m2+Ramucirumab10mg/kg(Ramucirumab组)、多西他赛75mg/m2+安慰剂(对照组),每三周接受一次用药。要求入选对象为复发或转移性乳腺癌患者,且尚未接受细胞毒性化疗或生物治疗。如患者出现癌症进展、难以忍受的毒副作用等退出标准即停止试验。中位随访时间为18.6个月。
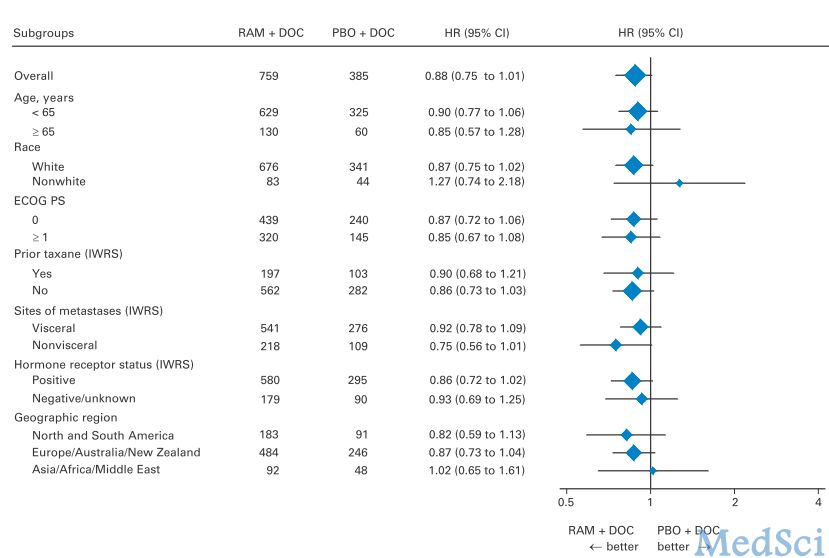
将患者按照紫杉醇治疗史、内脏转移、激素受体及地域情况进行亚组分析,主要结局变量为无进展生存期(progression-free survival,PFS)。
结果显示,Ramucirumab组无进展生存期的中位数为9.5个月,对照组为8.2个月,风险比(hazard ratio,HR)=0.88,P=0.077。Ramucirumab组总生存期中位数为27.3个月,对照组为27.2个月,HR=1.01,P=0.915。Ramucirumab组的的无进展生存期和总生存期均有大于对照组的趋势,但均无统计学意义。亚组分析结果也是一样,见图1。Ramucirumab组出现的较明显的副作用有疲乏、高血压、发热性中性粒细胞减少、肢端红肿症(palmar-plantar erythrodysesthesia syndrome,PPE综合症)及口腔炎。
可见,Ramucirumab与紫杉醇联合用于HER2阴性的进展期乳腺癌患者,对关键的临床结局无改善作用。
Ramucirumab是Lily公司开发的血管内皮生长因子(VEGF)2型受体单抗,2014年4月FDA批准其上市,批准的适应症为化疗失败的胃癌、胃食管连接处腺癌,无乳腺癌。
原始出处:
本文是MedSci原创编译整理,欢迎转载!转载请注明来源并附原文链接。谢谢!

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#临床结局#
42
#mAb#
36
#JCO#
36
it's not good to woman
106
#转移性#
31
#Ramucirumab#
42
Ramucirumab单抗非常火呀
100