JAMA Neurol:质子泵抑制剂增加痴呆风险
2016-02-21 Mechront 译 MedSci原创
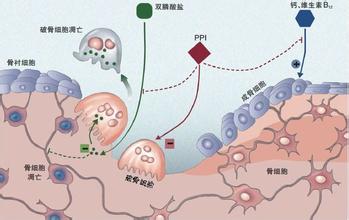
近期发表在JAMA Neurology的研究称,使用质子泵抑制剂(PPI)可能会增加痴呆风险。PPI是使用最广的药物之一,近年来老年人PPI的使用也在增加。德国神经退行性疾病中心的Britta Haenisch博士和同事对2004-2011年间的数据进行了分析,探究PPIs的使用和痴呆风险间的联系。规律使用PPI定义为至少每隔18个月就有一张PPI的处方。最终73,679名≥75岁的人群数据用于了
德国神经退行性疾病中心的Britta Haenisch博士和同事对2004-2011年间的数据进行了分析,探究PPIs的使用和痴呆风险间的联系。规律使用PPI定义为至少每隔18个月就有一张PPI的处方。
最终73,679名≥75岁的人群数据用于了分析,随访期间有29,510名患者发展为痴呆。研究数据显示,2,950名规律使用PPIs的患者(绝大多数为女性,平均年龄接近84岁)与没使用PPI的患者(70,729人,绝大多数为女性,平均年龄83岁)相比,痴呆风险高44%。
该研究的限制包括,作者只能从数据中纳入其他一些痴呆危险因素进行数据分析,对混杂因素的分析存在不全面的可能性。
研究总结道,目前的研究只能提供使用PPI和痴呆症风险之间的统计关联。在未来的研究中,将对可能存在的潜生物机制进行探讨,评估和建立PPI的使用与在老年人痴呆间的直接和因果关系,在以后随机、前瞻性临床试验是必要的。
原始出处:
Willy Gomm, Klaus von Holt, Friederike Thomé, Karl Broich, Wolfgang Maier, Anne Fink, Gabriele Doblhammer, Britta Haenisch. Association of Proton Pump Inhibitors With Risk of Dementia. JAMA Neurology, 2016.
Proton pump inhibitors may be associated with increased risk of Dementia
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#抑制剂#
27
#质子泵#
35
#Neurol#
42
希望有进一步的研究
127
多学点
54
#痴呆风险#
31
j
133
这
129
改
97
我
47