European Radiology:卷积神经网络在脑转移瘤自动检测中的应用
2022-04-06 shsaosai MedSci原创
利用深度学习技术(如神经网络)算法对脑转移瘤进行自动检测已引入临床应用。
 由于脑转移存在与否涉及到分期和治疗计划,因此对于脑转移瘤的准确诊断对于确定适当的治疗策略至关重要。例如,全脑放疗是多发转移的标准治疗方法;但对于病灶较小且较少的患者,则考虑采用立体定向放射治疗。因此,术前准确评估病灶的数量、大小以及位置至关重要。
由于脑转移存在与否涉及到分期和治疗计划,因此对于脑转移瘤的准确诊断对于确定适当的治疗策略至关重要。例如,全脑放疗是多发转移的标准治疗方法;但对于病灶较小且较少的患者,则考虑采用立体定向放射治疗。因此,术前准确评估病灶的数量、大小以及位置至关重要。
近年来,利用深度学习技术(如神经网络)算法对脑转移瘤进行自动检测已引入临床应用。一些研究已经证明了使用各种卷积神经网络(CNN)自动检测脑转移瘤的优势。在强化后的T1加权成像中,增强的血管可能被误诊为转移性肿瘤。因此,人们引入了血管抑制的成像方法来减少假阳性(FPs)的发生。有学者提出了一种三维MR序列-VISIBLE技术,用于脑转移瘤的检测。VISIBLE可同时采集有血管抑制的图像(以下简称 "黑图像")和没有血管抑制的图像("亮图像")。
近日,发表在European Radiology杂志的一项研究开发了一项使用CNN和VISIBLE检测脑转移瘤的自动模型,并将其诊断性能与之前的观察者测试进行了比较,为脑转移瘤快速准确的定量、定性及定位提供了技术支持。
本项回顾性研究纳入了2016年3月至2019年7月采用VISIBLE成像的临床怀疑有脑转移的患者。选取有和无血管抑制的图像用于训练现有的CNN(DeepMedic)。使用灵敏度和每个病例的假阳性结果(FPs/case)评估了诊断性能。本研究将CNN模型的诊断性能与12位放射科医生的诊断性能进行了比较。
本研究将50名在随访中被临床诊断为脑转移的患者(30名男性和20名女性;年龄范围29-86岁;平均63.3±12.8岁;共165个转移病例)用于训练。本研究提出模型的敏感性为91.7%,并高于观察者测试(平均±标准差;88.7±3.7%)。模型中的FPs/病例数为1.5,并高于观察者测试(0.17±0.09)。
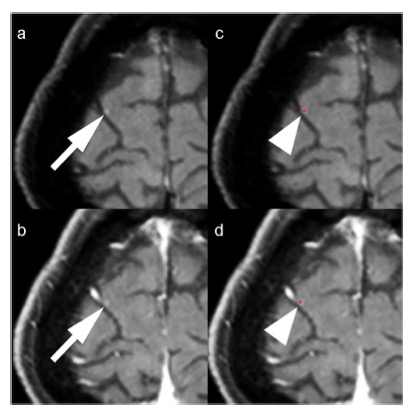
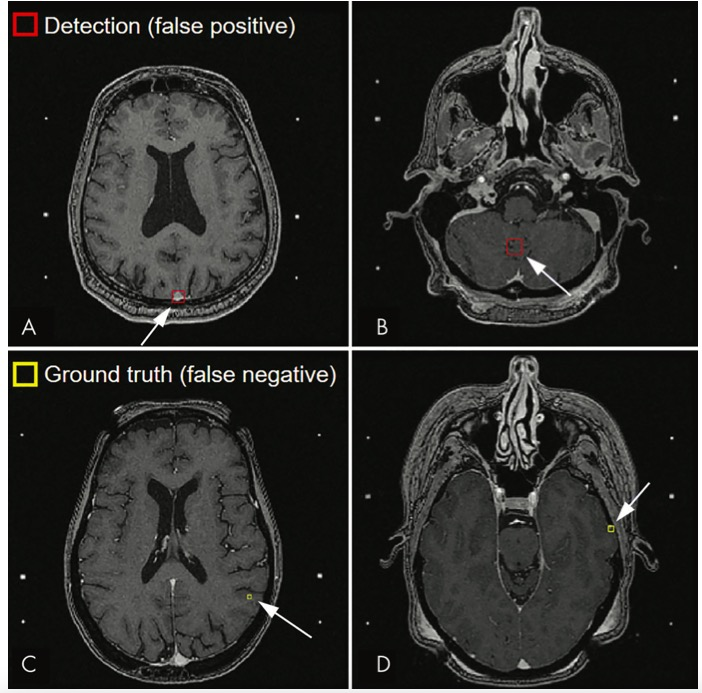
图 60岁的女性,患有肺癌和多个脑转移病变。在黑(a)和亮(b)图像中,显示右侧额叶一个转移瘤(箭头)。其大小约为2毫米。我们的CNN模型在黑(c)和亮(d)图像中准确地检测到这个病灶(箭头)
总之,与放射科医生相比,本研究由VISIBLE和CNN创建的诊断脑转移的模型显示出了更高的灵敏度。
原文出处:
Yoshitomo Kikuchi,Osamu Togao,Kazufumi Kikuchi,et al.A deep convolutional neural network-based automatic detection of brain metastases with and without blood vessel suppression.DOI:10.1007/s00330-021-08427-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#PE#
33
#转移瘤#
31
#脑转移瘤#
54
#神经网络#
41