JAMA Dermatol:用双光子荧光显微镜实时分析皮肤活检标本
2022-09-14 紫菀款冬 MedSci原创
验证非黑色素瘤皮肤癌(NMSCs)的双光子荧光显微镜(TPFM)成像是否可以在获得活检样本后几分钟内发生,并提供与常规组织学相似的组织学特征,评估TPFM相对于常规组织学的诊断性能。
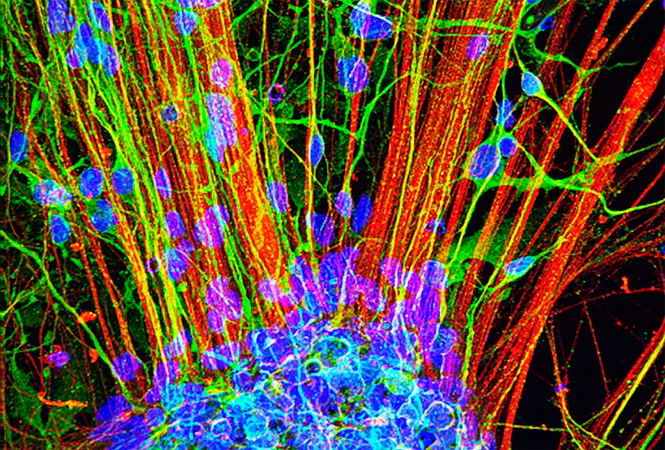
背景:非黑色素瘤皮肤癌(NMSCs)主要通过皮肤活检标本的石蜡切片组织学分析进行诊断,但是往往需要几天到几周才能出局正式的诊断报告。双光子荧光显微镜(TPFM)有可能用于NMSC和其他皮肤疾病的即时检测诊断,一次就诊就可以实现诊断和治疗。
目的:证明NMSC的TPFM可以在几分钟之内获得成像结果,并提供与常规组织学相似的组织学特征,评估TPFM相对于常规组织学的诊断性能。
方法:该项比较有效性的试点研究检查了29例新切除的活检样本,这些样本来自接受治疗的患者中确诊的NMSC病变。2019年10月至2021年8月,在罗切斯特皮肤外科(Victor, New York)现场用TPFM立即对活检样本进行成像。随后,将成像活检提交石蜡组织学检查,生成同部位的图像。
这些共配准图像对中的12对(41.4%)被用作训练集。15个样本(51.7%)被委员会认证的皮肤病理学家用于掩盖评估。2个样本(6.9%)因为无法共同登记,在评估前被排除在研究之外。
评估TPFM对NMSC活检的敏感性、特异性和准确性,并与常规组织学进行比较。
结果:评估组15例活检标本中有14例(93.3%)与TPFM和石蜡组织学诊断一致。TPFM诊断基底细胞癌的敏感性为100%(95%CI,48%-100%),特异性为100%(90%CI,69%-100%),准确性为100%(50%CI,78%-100%)。
对于鳞状细胞癌的诊断,TPFM具有89%的敏感性(95%CI,52%-100%)、100%的特异性(95%CI,54%-100%)和93%的准确性(95%CI,68%-100%)。
对于NMSC的总体诊断,TPFM具有93%的敏感性(95%CI,66%-100%)、100%的特异性(95%CI,3%-100%)和93%的准确性(95%CI,68%-100%)。对1个不配对样本的检查显示不匹配的成像平面是误差源。
结论:该项比较有效性试点研究的结果表明,TPFM捕获了传统组织学中存在的NMSC的组织学特征,显示了其作为一种快速、即时检测诊断替代方案的潜力,不需要大量的样本制备或图像评估的再培训。后续需要对更大队列进行进一步的TPFM成像验证,以充分评估其诊断准确性和在现场的潜在影响。
文献来源:
Ching-Roa VD, Huang CZ, Ibrahim SF, Smoller BR, Giacomelli MG. Real-time Analysis of Skin Biopsy Specimens With 2-Photon Fluorescence Microscopy [published online ahead of print, 2022 Sep 7]. JAMA Dermatol. 2022;10.1001/jamadermatol.2022.3628. doi:10.1001/jamadermatol.2022.3628
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#显微镜#
45
#标本#
32
#荧光#
34
#活检#
43
#皮肤活检#
0