拉肚子会让人变傻实锤了!Science:肠道炎症引起脑屏障结构改变,诱发精神症状!
2021-11-03 梅斯医学 MedSci原创
几乎每个人都有过这样的经历:腹内绞痛,伴随肠道蠕动带来咕噜噜的声响,“城门即将失守”的红色警报在脑海高分贝鸣响,没有哪一刻像现在,注意力完全集中于一处,一只马桶,一个蹲坑,哪怕
几乎每个人都有过这样的经历:腹内绞痛,伴随肠道蠕动带来咕噜噜的声响,“城门即将失守”的红色警报在脑海高分贝鸣响,没有哪一刻像现在,注意力完全集中于一处,一只马桶,一个蹲坑,哪怕是一个草丛都行!
腹泻的绝望太深刻,特别是在高速路上,有一句话叫:闹肚子的时候,不要相信任何一个屁……一旦控制不住,视当下的场景,周围有多少人,按陌生人、亲人、朋友、暗恋对象等,给人的精神和视、听觉造成了不同程度的、难以磨灭的创伤。
如果这就让你绝望了,那些因为反复的腹泻和腹痛备受煎熬,严重到影响日常生活、工作和学习,并且病程迁延不愈,甚至持续终生的人又要如何生活?
他们就是炎症性肠病患者。
炎症性肠病(inflammatory bowel disease, IBD)是一种病因不明的慢性非特异性炎性肠道疾病,主要包括克罗恩病和溃疡性结肠炎。流行病学资料显示,近年来我国IBD发病率呈快速上升趋势,患病人数已达3.44/100000,居亚洲首位。
炎症性肠病患者不止饱受腹痛腹泻之苦,研究显示,40%的IBD患者还伴有焦虑、抑郁症状,甚至产生认知功能受损。在结肠炎小鼠身上,同样能够观察到焦虑、抑郁行为产生以及大脑边缘系统的改变。但肠炎导致精神症状的机制还不清楚。
不同于大众认知层面简单地将IBD患者的焦虑和抑郁症状归因于疾病的痛苦,科学家将目光放在肠-脑联系上。近期发表在Science的一篇研究就从肠-脑血管轴入手,揭示了肠道炎症引起精神症状的关键机制。
我们知道,肠道炎症状态下,肠道血管屏障渗漏增加,肠腔内的细菌毒素也随之进入血液循环之中,引起系统性全身炎症反应。
由于中枢神经系统拥有复杂的血管屏障,包括血-脑屏障和血-脑脊液屏障,正常情况下,脑血管屏障会限制血液中的大分子物质进入脑内,维持脑组织内环境处于稳定状态。
但研究人员观察到,在小鼠结肠炎急性期,小鼠大脑中的巨噬细胞数量增加,同时,小胶质细胞,神经系统主要的免疫监视细胞也处于被激活状态,说明肠道炎症能够迅速引起脑部炎症反应。
那么,肠道炎症状态下,肠道来源的细菌毒素和血液中的炎症因子是如何进入脑内的呢?
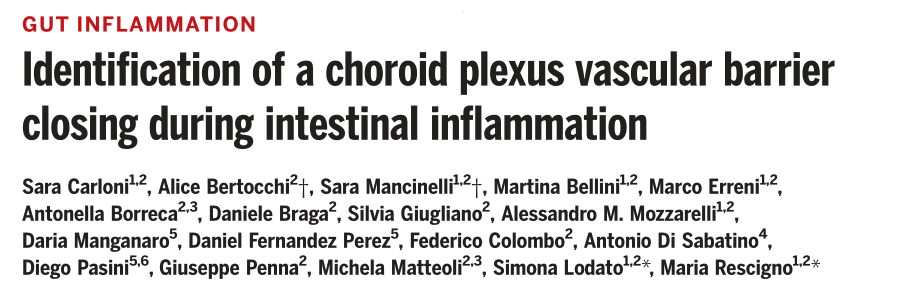
为此,研究人员分别在正常状态、急性肠炎期和肠炎恢复期向小鼠眼眶后静脉丛注射带有荧光探针的70KDa葡聚糖,观察脑血管屏障渗透性的变化。由于血-脑屏障仅能通过500 Da的脂溶性物质,因此,70KDa的荧光分子更有可能是通过血-脑脊液屏障进入脑内。
研究人员观察到,在急性肠炎第一天,脑血管屏障通透性增强,荧光分子聚集渗入到脑脉络丛区,在脑脊液中也能发现荧光分子存在,然而在肠炎第三天,荧光分子被完全阻挡在脑血管屏障之外,直到肠炎恢复后,荧光分子才能够再次进入脑内。
说明在急性肠炎状态下,脑血管屏障结构发生改变,尽管在初期脉络丛区脑血管屏障通透性一过性增强,随后,脑血管屏障迅速关闭,直到肠炎恢复,才重新开放。
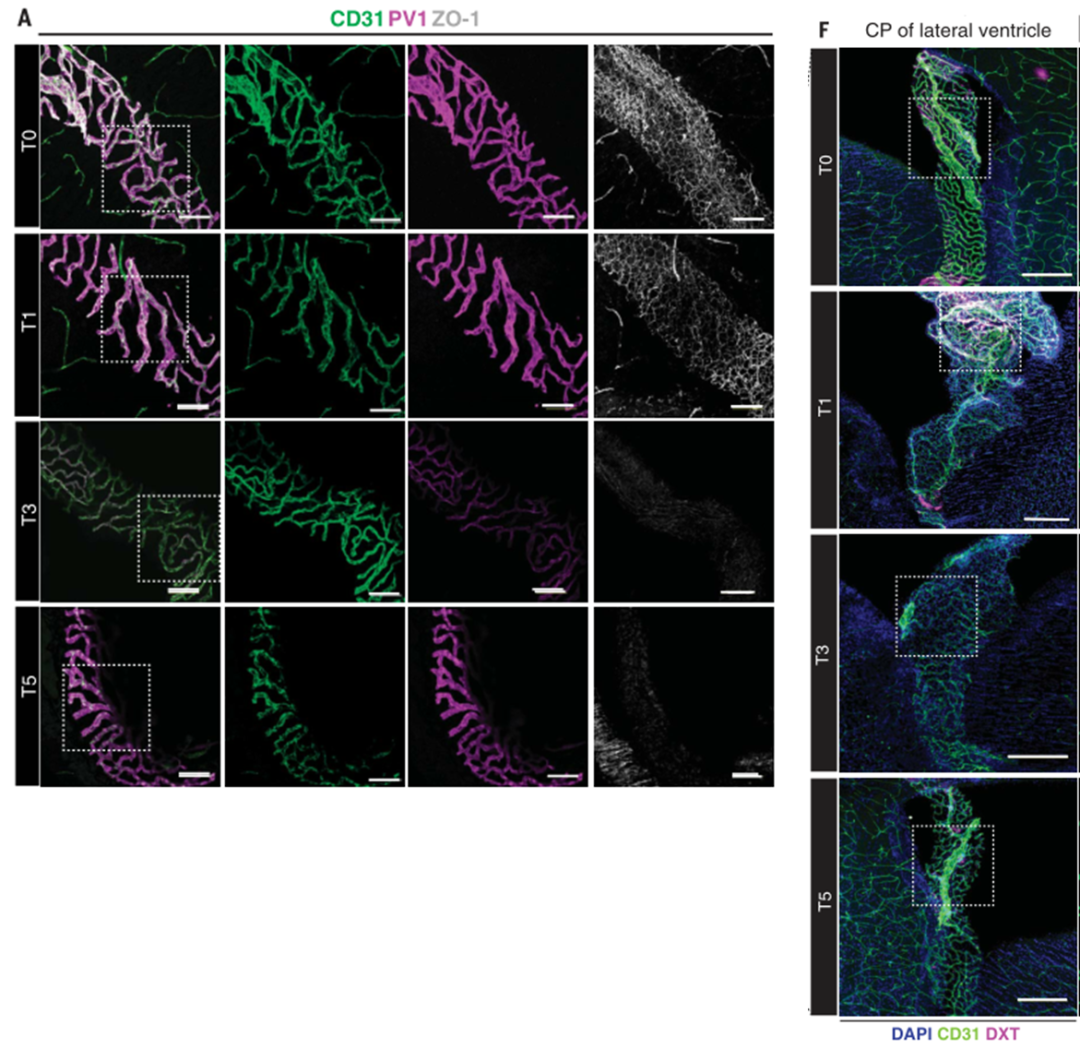
而向小鼠腹腔内注射细菌内毒素——脂多糖LPS,同样可以在小鼠脑部观察到类似急性结肠炎时发生的变化——脉络丛血-脑脊液屏障关闭,说明细菌内毒素的存在影响脑血管屏障结构改变。
研究进展到此,我们已经知道急性肠炎状态下,肠道血管屏障渗透性增加,肠内细菌产生的内毒素进入血液循环中,到达脑部,改变脑血管屏障结构,脑屏障关闭……
等等,好像和想象的有点出入,既然脑屏障关闭了,那么按理来说,有害物质不能进入脑部了,应该就不会对脑产生进一步影响,那么焦虑、抑郁,甚至认知下降是如何产生的呢?
难道因为急性肠炎第一天脑血管屏障渗透性增强循环中有害物质进入脑内导致的?还是天天腹泻使得小鼠和患者感到心情痛苦呢?
最妙的一步来了,研究人员设计了一种基因编辑小鼠在注射诱导药物后,能够使得小鼠在没有肠道炎症和疾病痛苦的情况下,脑血管屏障关闭,这时再去研究小鼠的行为。
研究人员发现脑血管屏障关闭后,小鼠出现了焦虑样行为、情景记忆能力受损,而抑郁行为则没有表现。原来精神症状,至少是部分精神症状出现的关键,就出在关闭的脑血管屏障!
到这里为止,所有的事件终于可以串起来了:在肠道炎症状态下,有害物质进入血液,脑血管屏障感受到了这种“威胁”,选择关闭来阻止有害物质进入,维持脑内稳态,然而隔绝了对外来往,有害物质不能进入,有益物质也不能进入,脑内产生的垃圾同样运不出去,这时就产生了就会产生精神症状。
最后,还是有问题遗留:尽管在小鼠身上关闭血管屏障后,我们只看到了焦虑样症状及认知功能下降,如果是长期反复地诱导关闭脑血管屏障,是否能够观察到抑郁症状呢?
其次,在动物模型上,研究人员观察到脑血管屏障的改变在肠炎恢复后也能回到原状,如果是长期的反复发作的肠炎,比如临床上的IBD患者,脑屏障结构的改变还是一过性的吗,是否会发生永久性的改变呢?这些问题还有待科学家进一步研究。
参考文献:
1.Ng, S.C., et al., Incidence and phenotype of inflammatory bowel disease based on results from the Asia-pacific Crohn's and colitis epidemiology study. Gastroenterology, 2013. 145(1): p. 158-165.e2.
2.Byrne, G., et al., Prevalence of Anxiety and Depression in Patients with Inflammatory Bowel Disease. Can J Gastroenterol Hepatol, 2017. 2017: p. 6496727.
3.Dempsey, E., et al., Persistent central inflammation and region specific cellular activation accompany depression- and anxiety-like behaviours during the resolution phase of experimental colitis. Brain Behav Immun, 2019. 80: p. 616-632.
4.Carloni, S., et al., Identification of a choroid plexus vascular barrier closing during intestinal inflammation. Science, 2021. 374(6566): p. 439-448.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#精神症状#
52
#拉肚子#
47
#SCIE#
37
#肠道炎症#
44
很有意思的文章
91