Lancet:双特异性抗体faricimab在湿性或新生血管性年龄相关性黄斑变性(AMD)和糖尿病性黄斑水肿(DME)1年的随访结果
2022-01-29 MedSci原创 MedSci原创
2022年1月24日,罗氏子公司基因泰克(Genentech)宣布,已经在《柳叶刀》上发表了两篇论文,重点介绍了双特异性抗体faricimab在湿性或新生血管性年龄相关性黄斑变性(AMD)和糖尿病性黄
2022年1月24日,罗氏子公司基因泰克(Genentech)宣布,已经在《柳叶刀》上发表了两篇论文,重点介绍了双特异性抗体faricimab在湿性或新生血管性年龄相关性黄斑变性(AMD)和糖尿病性黄斑水肿(DME)中的四项关键III期研究的一年结果。详细见:长效双特异性抗体faricimab用于特定黄斑变性和糖尿病性黄斑水肿,4个月注射一次,效果出色
治疗AMD
AMD是一种影响黄斑的疾病,是60岁及以上人群失明的主要原因。湿性或新生血管性AMD是该疾病的晚期形式,如果不及时治疗,可导致快速和严重的视力丧失。
TENAYA和LUCERNE是两项相同的、随机、多中心、双盲全球III期研究,在1329例(TENAYA为671例,LUCERNE为658例)湿性AMD患者中评估了faricimab与aflibercept相比的安全性和有效性。每个研究都有两个治疗组,faricimab治疗组又分为每8、12或16周间隔接受剂量为6.0 mg的faricimab治疗的三个队列,aflibercept治疗组则每8周接受一次剂量为2.0 mg的aflibercept治疗。主要终点是从基线到第48周的最佳矫正视力(BCVA)评分。
在湿性AMD的TENAYA和LUCERNE研究中,分别有46%和45%接受faricimab治疗的患者能够在第一年每四个月给药一次。另外分别有34%和33%的患者能够每三个月给药一次。综合来看,近80%接受faricimab治疗的患者在第一年的治疗间隔能够持续三个月或更长时间。
治疗DME
DME是糖尿病性视网膜病变(DR)的并发症,可引起失明。DR是由于血管受损以及在眼睛中形成新血管而导致血液和液体泄漏到视网膜中引起的。这会导致视网膜某些部位的肿胀和血液供应受阻。DME是指受损的血管渗入黄斑并引起肿胀。黄斑是视网膜的中央区域,负责阅读和驾驶所需的清晰视力。
两项代号为TENAYA (NCT03823287) 和LUCERNE (NCT03823300)的两项III期研究分别在671例和658例nAMD患者中评估faricimab和阿柏西普的疗效和安全性差异。
YOSEMITE和RHINE是两项相同的、随机、多中心、双盲全球III期研究,在1891例(YOSEMITE为940例,RHINE为951例)DME患者中评估faricimab与aflibercept相比的疗效和安全性。每项研究都有三个治疗组,一组每隔8周接受aflibercept的注射,一组每隔8周接受faricimab的注射,第三组接受个体化的faricimab注射频率,最长可间隔16周接受一次注射。研究的主要终点是一年后与基线相比BCVA评分的平均变化。
研究均设置faricimab 6mg(每2个月、3个月或者4个月1次,根据第20周和第24周疾病活动程度评估确定)和阿柏西普2mg(每2个月1次)两个给药组。研究的主要终点是第48周最佳矫正视力(BCVA)评分较基线的平均变化,次要终点包括安全性,faricimab 组每2个月、3个月或4个月1次的受试者比例,BCVA评分较基线增高和避免降低15个字母以上受试者比例,黄斑中心区视网膜厚度较基线的变化。
在DME的YOSEMITE和RHINE研究中,分别有53%和51%接受faricimab治疗的患者能够在第一年每四个月给药一次。另外分别有21%和20%的患者实现了三个月给药一次。综合来看,超过70%的接受faricimab治疗的患者在第一年结束时的治疗间隔能够持续三个月或更长时间。
结果显示,faricimab在治疗第48周的视觉敏锐度(BCVA评分)较基线的改善程度均不劣于阿柏西普,在TENAYA研究和LUCERNE研究中分别改善5.8和6.6个字母,而阿柏西普组为5.1和6.6个字母,到达了主要终点。
TENAYA研究中,faricimab治疗组nAMD患者在第1年时能够实现每4个月1次给药的比例为45.7%(144/315),每3个月1次给药的比例为34%(107/315);LUCERNE研究中,faricimab治疗组在第1年时能够实现每4个月1次给药的比例为44.9%(142/316),每3个月1次给药的比例为32.9%(104/316)。相当于接受faricimab治疗的患者近80%在1年时能够实现每3个月或更长时间间隔的注射给药。此外,每4个月1次faricimab在黄斑中心区视网膜厚度降低方面也不劣于每2个月注射1次阿柏西普。
2021年7月29日,美国FDA已授予faricimab的生物制品许可申请(BLA)优先审评资格,用于治疗湿性AMD和DME。一旦获批,faricimab将成为首个用于眼睛的双特异性抗体。
从雷珠单抗到长效给药装置(PDS),再到双特异抗体,再到基因治疗领域,罗氏持续领跑眼科治疗领域,有望为更多患者带来新的曙光。
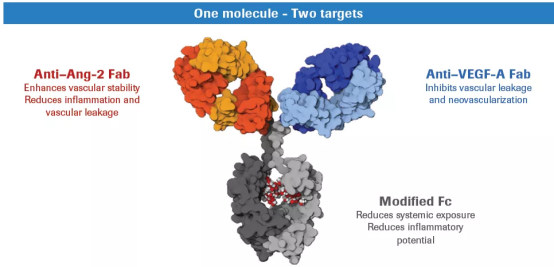
Faricimab同时靶向VEGF和Ang2信号通路
Faricimab是首个针对眼睛设计的在研双特异性抗体。它靶向血管生成素-2(Ang-2)和血管内皮生长因子-A(VEGF-A)两个不同的通路,Ang-2和VEGF-A通过破坏血管的稳定性导致新的渗漏血管形成并增加炎症,从而影响视力。通过阻断这两种通路,faricimab旨在稳定血管,长期为患有视网膜疾病的人改善视力。
原始出处:
Wykoff CC, Abreu F, Adamis AP, Basu K, Eichenbaum DA, Haskova Z, Lin H, Loewenstein A, Mohan S, Pearce IA, Sakamoto T, Schlottmann PG, Silverman D, Sun JK, Wells JA, Willis JR, Tadayoni R; YOSEMITE and RHINE Investigators. Efficacy, durability, and safety of intravitreal faricimab with extended dosing up to every 16 weeks in patients with diabetic macular oedema (YOSEMITE and RHINE): two randomised, double-masked, phase 3 trials.Lancet. 2022 Jan 21:S0140-6736(22)00018-6. doi: 10.1016/S0140-6736(22)00018-6.
Heier JS, Khanani AM, Quezada Ruiz C, Basu K, Ferrone PJ, Brittain C, Figueroa MS, Lin H, Holz FG, Patel V, Lai TYY, Silverman D, Regillo C, Swaminathan B, Viola F, Cheung CMG, Wong TY; TENAYA and LUCERNE Investigators.Efficacy, durability, and safety of intravitreal faricimab up to every 16 weeks for neovascular age-related macular degeneration (TENAYA and LUCERNE): two randomised, double-masked, phase 3, non-inferiority trials.Lancet. 2022 Jan 21:S0140-6736(22)00010-1. doi: 10.1016/S0140-6736(22)00010-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#新生血管性年龄相关性黄斑变性#
0
#Lancet#
37
#随访结果#
66
#特异性#
28
#血管性#
36
#mAb#
26
#新生血管#
40
#相关性#
34
#年龄相关#
37
#DME#
36