Chest:MRSA肺炎预后因素
2015-11-12 徐媛 MedSci原创
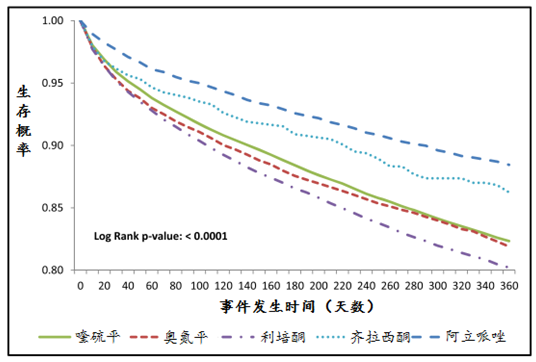
研究人员通过用ICD-9-CM 编码482.42确认来自2009-2011年全美住院病人样本数据库的MRSA肺炎患者,并研究了死亡率,住院时间(LOS)以及急性呼吸窘迫综合征(ARDS)预后因素。研究人员还分析了受试者年龄、性别或者Charlson发病率指数(CCI)是否对以上三个预后结果产生影响。使用逻辑回归评估ARDS的优势比和死亡率。 研究人员共收纳来自2009-2011年44372名MR
研究人员通过用ICD-9-CM 编码482.42确认来自2009-2011年全美住院病人样本数据库的MRSA肺炎患者,并研究了死亡率,住院时间(LOS)以及急性呼吸窘迫综合征(ARDS)预后因素。研究人员还分析了受试者年龄、性别或者Charlson发病率指数(CCI)是否对以上三个预后结果产生影响。使用逻辑回归评估ARDS的优势比和死亡率。
研究人员共收纳来自2009-2011年44372名MRSA肺炎患者,MRSA肺炎的总死亡率为13.9%。住院时间大于20天患者占20.4%。MRSA肺炎患者占ARDS患者总数的0.8%。CCI的影响:CCI每增加1的ARDS的优势比OR为0.98 (95%CI 0.92-1.04, p value 0.49), 死亡率的优势比OR为1.10 (95%CI 1.08-1.11, p value <0.0001),LOS的优势比OR为1.01 (95%CI 1.004-1.013, p value 0.0002)。年龄的影响:年龄每提高10岁,ARDS的优势比为0.92 (95%CI 0.86-0.98, p value 0.0084),死亡率的优势比OR为 1.20 (95%CI 1.18-1.23, p value <0.0001),LOS的优势比OR为 0.96 (95%CI 0.956-0.968, p value <0.001)。性别的影响:以男性为基线,ARDS的优势比为0.97 (95%CI 0.78-1.19, p value 0.75),死亡率的优势比为 0.86 (95%CI 0.81-0.91, p value <0.0001),LOS的优势比为0.95 (95%CI 0.938-0.969, p value <0.0001)。
以上研究结果,MRSA肺炎死亡率为13.9%。年龄、性别以及CCI均可以影响MRSA肺炎死亡率。年龄每提高10岁,死亡率提高20%。CCI每提高1,死亡率提高10%。女性比男性死亡率低14%。仅仅年龄对MRSA肺炎患者是否发生ARDS有影响。年龄每提高10岁,ARDS的发生率降低8%。对于住院时间,年龄每提高10岁,住院时间缩短4%;女性住院时间较男性缩短5%;CCI每提高1,住院时间延长1%。在合并多种并发症的老年患者中MRSA肺炎的死亡率更高。MRSA肺炎患者是否发生ARDS与并发症无关,与年龄呈负相关。女性患者死亡率更低,住院时间更短。
原始出处
Saqib Baig, MD; Ezza Khan, MD; Aniko Szabo, PhD; Nicholas DeVogel.Outcomes of Methicillin Resistant Staphylococcus aureus (MRSA) Pneumonia in Adult Patients (>18 Years).Chest.2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#EST#
28
继续学习
57
继续关注
46
#mRS#
33
#Chest#
31
这篇文章有一定深度
162
是一篇不错的文章
136
#MRSA#
36
#预后因素#
25
赞
121