Cardiovasc Diabetol:无症状T2D患者高危冠状动脉斑块的发生率及相关风险因素
2021-08-10 Nebula MedSci原创
无症状T2D患者高危冠状动脉斑块的发生率较高,男性、烟龄和糖化血红蛋白都是其风险因素
急性心肌梗死(MI)主要由冠状动脉斑块破裂和冠状动脉闭塞引起的。破裂斑块的特征是脂质丰富,正性重构(PR)面覆盖了一层由炎症细胞浸润的纤维帽。高危型冠状动脉斑块(HRP)与急性冠状动脉综合征的风险增加相关。
本研究旨在调查无症状2型糖尿病(T2D)患者的HRP发生率,及其与患者心血管危险因素、糖尿病状况和冠状动脉钙评分(CACS)等患者特征的关系。
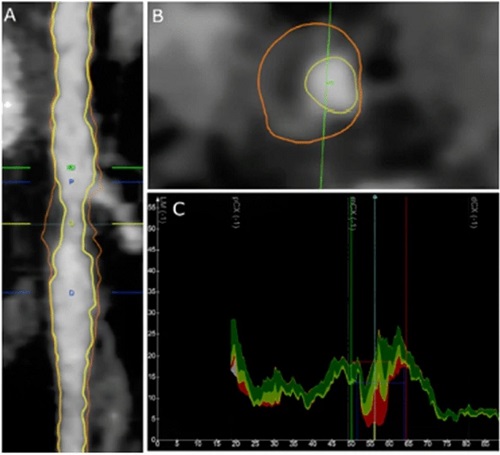
研究人员采用冠状动脉CT血管造影(CCTA)对既往无冠状动脉疾病(CAD)史的无症状T2D患者进行评估。具有低衰减、正性重构、点状钙化和餐巾环征的两种或两种以上高危特征的斑块被认为是HRP。此外,还评估了总动脉粥样硬化体积(TAV),致密钙化、纤维化、纤维脂肪和坏死核心体积的比例。最后,还评估所有患者的心血管和糖尿病情况。
斑块检测示例
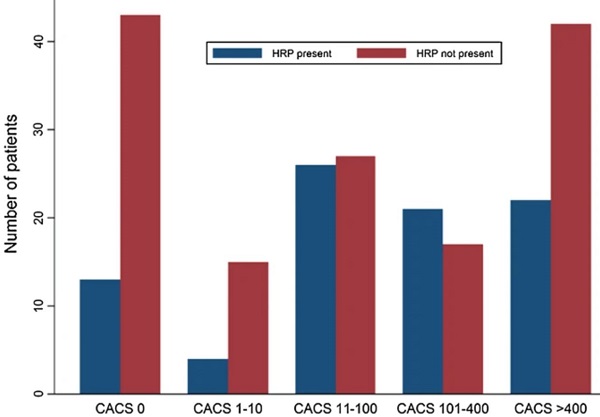
共有230位患者进行了诊断性的CCTA,在其中86位(37%)患者中检出了161处HRP。男性(OR 4.19, 95%CI 1.99-8.87; p<0.01)、烟龄(OR 1.02, 95%CI 1.00–1.03; p=0.03)和糖化血红蛋白(HbA1c:OR 1.04, 95%CI 1.02–1.07; p<0.01)都是HRP的独立预测因素。其他风险因素未发现与HRP存在相关性。HRP与CACS升高无相关性,12位(23%)CACS评分 0分的患者至少有一处HRP。
根据CACS分层的患者HRP发生率
综上所述,HRP在无症状T2D人群中发生率较高。HRP的存在与特定的患者情况有关;此外,动脉钙化缺乏不能排除HRP的存在。CCTA提供了斑块形态的重要信息,可用于对高危人群进行风险分层。
原始出处:
Heinsen, L.J., Pararajasingam, G., Andersen, T.R. et al. High-risk coronary artery plaque in asymptomatic patients with type 2 diabetes: clinical risk factors and coronary artery calcium score. Cardiovasc Diabetol 20, 164 (2021). https://doi.org/10.1186/s12933-021-01350-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#BET#
34
#冠状动脉斑块#
46
#DIA#
26
#发生率#
34
#ASC#
36
#斑块#
0
#无症状#
30
学习了
49