肿瘤治疗电场为复发性卵巢癌患者带来新希望,无进展生存期延长两倍!
2017-10-24 佚名 全球肿瘤医生网
一项重磅2期临床试验致力于研究肿瘤治疗电场(下文简称为“TTFields”)在结合每周一次紫杉醇时对于复发性卵巢癌的疗效。美国癌症研究协会将亲自见证这一结果。
该研究是一项前瞻性的单臂创新研究,以探究TTFields在治疗复发性卵巢癌的可行性、安全性和初步疗效。
研究发现,接受TTFields治疗的患者,无进展生存期(PFS)延长至8.9个月(而对照组患者PFS仅为3.9个月),显着延长了患者生命。但有小部分患者表现为铂类耐药性,治疗对复发性卵巢癌无效。目前尚未发现严重不良事件,仅两例患者出现严重皮肤过敏。
研究人员认为,基于复发性卵巢癌的难治愈性,目前针对TTFields的研究结果给治疗带来了希望。与其他癌症疗法结合使用时,TTFields能显着增加患者生存率,而不会使副作用明显增加。目前关键是要发展第三阶段试验,以进一步明确TTFields在治疗复发性卵巢癌方面的前景。
美国食品和药物管理局目前尚未批准TTFields针对卵巢癌的治疗方案。未来TTFields治疗卵巢癌的安全性和有效性有待进一步确证,以期给卵巢癌患者带来生存希望。
FDA已批准的适应症有哪些
美国FDA批准Optune治疗初诊脑胶质瘤患者
常规脑胶质瘤治疗手段包括:
· 外科手术: 手术尽可可能干净的清除体内的肿瘤细胞,并搞清楚肿瘤类型。
· 放疗:手术后可能需要放疗,医生可以使用高能x射线,伽马射线或者质子射线消灭体内的肿瘤学I包。
· 化疗: 医生可以使用药物杀死癌细胞,最常用的是替莫挫胺。
2015年美国FDA批准Optune治疗初诊脑胶质瘤患者
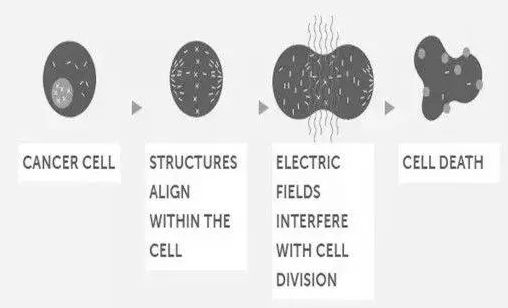
电场治疗(TTFields):电场治疗可以与化疗(替莫挫胺)联合使用,电场治疗可以减慢或者停止癌细胞分裂生长,也可能会导致癌细胞死亡。
TTFields (Optune)有更好的五年生存率
一项大型临床研究已经证明接受TTFields (Optune)联合替莫挫胺治疗比单独接受替莫挫胺化疗的生存期更长。TTFields (Optune)联合替莫挫胺治疗5年生存率13%,而单纯替莫挫胺化疗的5年生存率只有5%。
接受TTFields (Optune)联合替莫挫胺化疗的患者,接近一半生存期超过2年,而单独接受替莫挫胺化疗的患者,只有31%的患者超过2年。
2011年FDA批准Optune治疗复发脑胶质瘤
对于复发脑胶质瘤患者,一项大型临床研究已经证明TTFields (Optune)和化疗一样有效,使用TTFields (Optune)治疗和使用化疗治疗的患者,中卫生存期都是6个月左右,但是TTFields (Optune)患者有更好的生活质量。
生活质量
与接受化疗的患者比较,接受Optune电场治疗的患者报告有更好的生活质量,精神和认知功能都有提高。
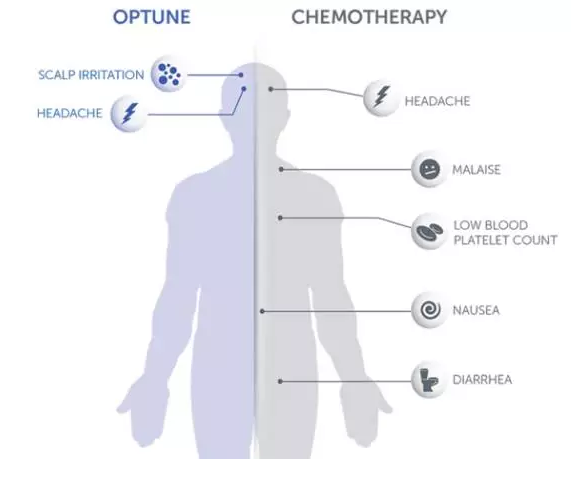
副作用
临床试验中,单独接受Optune治疗的患者报告的最常见的副作用(10%)是头皮刺激症状和头疼,没有化疗常见的副作用。而化疗的副作用为血小板降低,恶心,便秘,呕吐,疲乏,头疼等。
下图是Optune电场治疗和化疗引起的副作用的对比:
正在进行临床试验的癌症种类
科学家已经对电场治疗杀死癌细胞的机制有了更深入的了解,研究已经证明电场治疗(TTFields)对超过15种实体肿瘤细胞有抗有丝分裂作用,包括一些最具侵袭性的癌症。科学家正在开展电场治疗针对各种癌症的临床实验研究。
正在进行临床实验
卵巢癌:在一项针对复发卵巢癌的二期临床中,招募31位晚期铂类化疗失败的卵巢癌患者,使用TTF联合紫杉醇,临床数据显示患者的中位无进展生存期PFS高达8.9个月,而单药紫杉醇的PFS的历史数据只有3.9个月。
胰腺癌:一项针对晚期胰腺癌的二期临床中,招募20位没有化疗或者放疗过的晚期胰腺癌患者,采用TTF联合紫杉醇和吉西他滨进行治疗,这20位患者的中位无进展生存期达到12.7个月,而紫杉醇和吉西他滨联合吉西他滨的历史数据是5.5个月,表明TTF可能会让患者受益,不过这个临床没有对照组,只是历史数据的比对,后续还需要大规模的临床试验证实。
目前,这项最新的抗癌技术还未在国内开展。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#新希望#
37
#复发性#
34
#肿瘤治疗#
34
#复发性卵巢癌#
32
#生存期#
23
#无进展生存期#
29