Cardiovasc Diabetol:1型糖尿病患者的动脉僵硬度情况及其对心血管事件的预测价值
2022-06-13 MedSci原创 MedSci原创
大部分没有已知心血管疾病的长病程T1D患者表现出了过早的动脉硬化
动脉僵硬度是1型糖尿病 (T1D) 患者心血管疾病 (CVD) 风险的潜在生物标志物。但是,动脉僵硬度与其他心血管风险评估工具在T1D患者中的关系尚未阐明。该研究旨在评估无已知心血管疾病的T1D患者的动脉僵硬度,同时比较其与其他心血管风险评估工具在T1D患者中的实用性。
这是一项横断面研究,受试患者的T1D病程至少持续了10年,且无已知心血管疾病。根据2019年欧洲心脏病学会 (ESC) 指南,将受试患者分成不同的心血管疾病风险组,STENO T1D 风险引擎用于估计心血管事件的10年风险。通过颈股动脉脉搏波速度 (cf-PWV) 评估动脉僵硬度。评估冠状动脉钙(CAC)评分并进行颈动脉超声检查。此外,还评估了24小时动态血压和中心血流动力学参数。最后检索了有关肾功能和糖尿病肾病的数据。
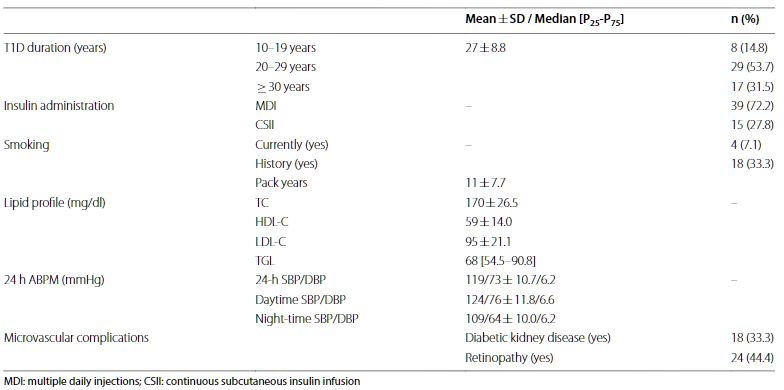
受试患者特征
共纳入了54位患者(46±9.5岁,T1D病程:27±8.8年)。根据cf-PWV,四分之一的患者存在主动脉僵硬度过早增加(24%)。Cf-PWV与CAC评分、颈动脉内膜中层厚度、中心血流动力学参数和糖尿病肾病显著相关。根据STENO,有低、中、高10年心血管事件风险的患者占比分别是37%(20位)、37%(10位)和14位(26%)。
Cf-PWV与STENO T1D CV事件风险评分的线性关系
Cf-PWV与STENO评分密切相关(rs=+0.81;R2=0.566,p<0.001),随着每个更高的STENO组而增加(p<0.01)。但是,根据ESC标准,在高和非常高心血管风险的两组中,cf-PWV无显著差异;与STENO标准相比,ESC标准划分的10年心血管事件风险>10%的患者多了10位(44/54 vs 34/54)。
总之,该研究显示,大部分没有已知心血管疾病的长病程T1D患者表现出了过早的动脉硬化。Cf-PWV与与未来发生心血管事件的STENO风险评分以及心血管成像和功能结果密切相关,说明了动脉僵硬度的临床重要性。但是,这些数据也显示出了心血管风险的显著异质性以及STENO工具和ESC标准之间风险分类的差异。
原始出处:
Helleputte, S., Van Bortel, L., Verbeke, F. et al. Arterial stiffness in patients with type 1 diabetes and its comparison to cardiovascular risk evaluation tools. Cardiovasc Diabetol 21, 97 (2022). https://doi.org/10.1186/s12933-022-01537-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ASC#
38
#BET#
34
#血管事件#
49
#1型糖尿病患者#
45
#DIA#
40
#糖尿病患者#
39
#动脉僵硬#
44
#动脉僵硬度#
54
#预测价值#
38