本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
2017-06-22 zhangfan MedSci原创
痤疮抗生素耐药性研究及治疗指南

这有点像双重人格者。在某个时刻,皮肤上的细菌是无害的,而下一刻,它们正在全面引发斑点状的粉刺。如今,研究人员发现了这一切是如何发生的。而该突破或许有望在两年内催生新的痤疮治疗方法。相关成果日前发表于《科学—免疫学》杂志。 来自美国加州大学圣地亚哥分校的Richard Gallo和同事发现,当一种生活在皮肤表面的无害细菌发现自己困在诸如毛囊等缺少空气的油性环境中时会变“坏”,从而触发炎
尽管80%的人经历过某一时期脸上长满痤疮的噩梦,但科学家仍未发现引发原因及阻止痤疮的方法。
这有点像双重人格者。在某个时刻,皮肤上的细菌是无害的,而下一刻,它们正在全面引发斑点状的粉刺。如今,研究人员发现了这一切是如何发生的。而该突破或许有望在两年内催生新的痤疮治疗方法。相关成果日前发表于《科学—免疫学》杂志。来自美国加州大学圣地亚哥分校的Richard Gallo和同事发现,当一种生活在皮肤表面的无害细菌发现自己困在诸如毛囊等缺少空气的油性环境中时会变“坏”,从而触发炎症和粉刺。缺少空
本文为欧洲痤疮循证治疗指南的简短版本,主要内容涉及痤疮诱导治疗,粉刺性痤疮的治疗,丘疹脓疱型痤疮的治疗,严重结节性/成团粉刺性痤疮的治疗和维持治疗的相关建议。全文获取:
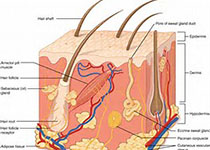
痤疮俗称“青春痘”“粉刺”,是多种因素导致的毛囊皮脂腺慢性炎症性皮肤病,多发于青少年。据统计,年龄在12岁至24岁之间的青年人中85%有痤疮,且可持续到成年。痤疮可能会导致焦虑、抑郁及皮肤永久疤痕等各种不良后遗症。这里小M整理了2016年以来关于痤疮的重要指南及共识以及重要研究与大家分享。【1】加拿大更新痤疮治疗指南最新一期的《加拿大医学协会期刊》根据加拿大皮肤专家的最新临床实践,对已沿用15


梅斯医学MedSci APP
医路相伴,成就大医
谢谢了,已学习
42
#治疗指南#
33
#抗生素耐药#
35
#抗生素耐药性#
36
学习了感谢分享
67