Clin Cancer Res:瑞博西尼联合多西他赛治疗转移性去势抵抗性前列腺癌
2022-02-22 Nebula MedSci原创
瑞博西尼联合多西他赛治疗转移性去势抵抗性前列腺癌显示出了可接受的毒性和令人鼓舞的疗效。
Ribociclib(瑞博西尼),是一种CDK4/6抑制剂,已被证实与紫杉烷类药物联合使用时具有临床前抗肿瘤活性。本研究是一项Ib/II期临床试验,旨在评估瑞博西尼联合多西他赛用于转移性去势抵抗性前列腺癌(mCRPC)患者的疗效和安全性。
招募了未进行过化疗的、经雄激素受体信号抑制剂(ARSI)治疗≥1次后进展的mCRPC患者。II期阶段的主要终点是6个月无影像学进展生存(rPFS)率(预计与对照相比是 55% vs 35%)。此外,还在基线时收集循环肿瘤细胞(CTC) 进行基因组分析。
共招募了43位患者(II期30位)。研究期间观察到了两例剂量限制性毒性(1例4级中性粒细胞减少症,1例4级发热性中性粒细胞减少症)。推荐的2期研究剂量(PR2D)和用药方案是多西他赛 60 mg/m2(21天一疗程)+瑞博西尼 400 mg/天(第1-4天和第8-15天)和非格司亭(第5-7天)。
受试患者的总rPFS率
使用推荐的2期研究剂量时,最常见的大于等于3级的副反应是中性粒细胞减少症(37%);但是,没有观察到发热性中性粒细胞减少症。主要终点达成;6个月rPFS率为65.8%(p=0.005),中位rPFS是8.1个月。32%的可评估患者获得了PSA50缓解。
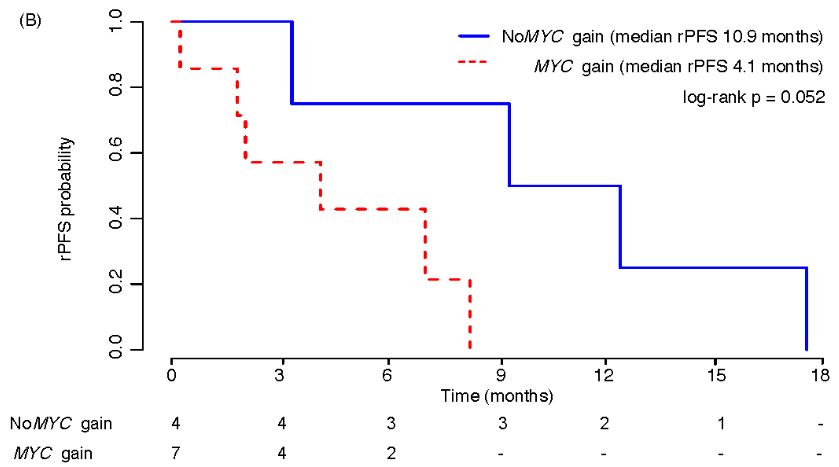
有无MYC扩增患者的rPFS率
最后,基线循环肿瘤细胞不携带MYC扩增与更长的rPFS相关(p=0.052)。
综上所述,间断性予以瑞博西尼加上每三周一次的多西他赛联合治疗ARSI预处理过的转移性去势抵抗性前列腺癌,显示出了可接受的毒性和令人鼓舞的疗效。循环肿瘤细胞基因谱或有助于识别最可能从该方案中获益的患者。该方案值得进一步开展随机临床试验进行验证。
原始出处:
Ivan de Kouchkovsky, Arpit Rao, Benedito A. Carneiro, Li Zhang, Catriona Lewis, Audrey Phone, Eric J. Small, Terence Friedlander, Lawrence Fong, Pamela L. Paris, Charles J. Ryan, Russell Z. Szmulewitz, Rahul Aggarwal; A phase Ib/II study of the CDK 4/6 inhibitor ribociclib in combination with docetaxel plus prednisone in metastatic castration-resistant prostate cancer. Clin Cancer Res 2022; clincanres.4302.2021. https://doi.org/10.1158/1078-0432.CCR-21-4302.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#抗性#
49
学习
45
#去势抵抗性前列腺癌#
39
#转移性#
40
受益匪浅
51