Neurology:及早识别脑淀粉样血管病患者的脑叶出血,简化爱丁堡CT标准准确且实用!
2022-04-04 Naomi MedSci原创
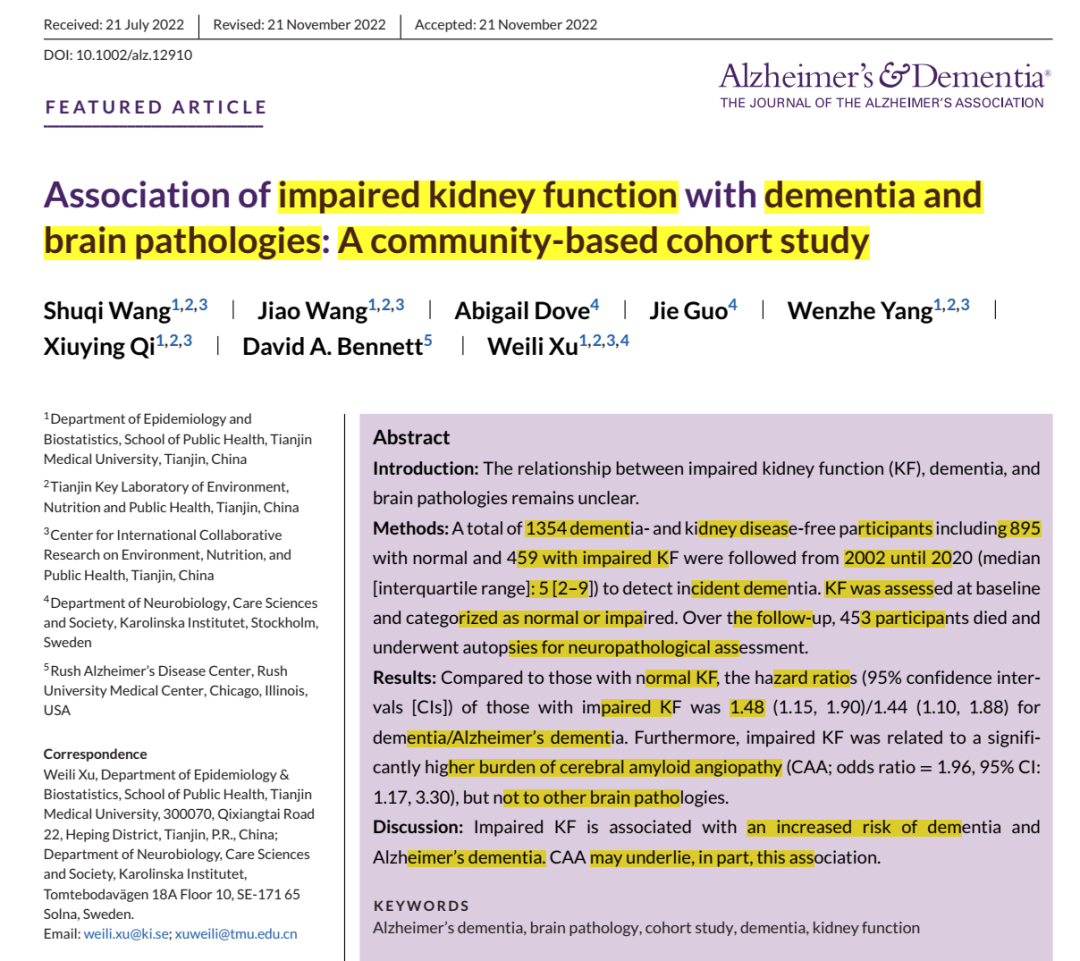
近日,研究人员调查了简化的爱丁堡 CT 标准在识别潜在的脑淀粉样血管病 (CAA) 方面的准确性和临床实用性。 这项研究提供了Ⅱ类证据,在大出血患者中,简化的爱丁堡标准准确地识别了那些高风险的CAA。
对于急性期和长期治疗来说,脑内出血(ICH)的诊断是关键的一步。高血压性脑小血管疾病是最常见的病因诊断,然而在脑叶脑出血中,评估出血病因则是一个更具挑战性的任务。对于后者,一个普遍的诊断代表散发性脑淀粉样血管病(CAA),增加至少一倍的重复发作风险。因此,关于长期管理的决策,特别是对于需要抗血栓预防的患者,通常是具有挑战性。此外,继发性原因,如动静脉畸形、海绵状血管瘤、动脉瘤或肿瘤,可能需要更具体的急性治疗策略。
CAA 体内诊断的现行标准代表 MRI 具有血液敏感序列,用于检测脑微出血和皮质浅表铁质沉着症(通过修改后的波士顿标准评估)。2018 年,罗德里格斯等人首次描述了诊断 CAA 相关性大叶 ICH 的极具鉴别力的爱丁堡标准,即非对比 CT 数据,包括存在蛛网膜下腔出血 (SAH) 和血肿的手指样投射,以及基因检测,包括 APOE ε4 拥有。已经提出了一种简化的仅 CT 模型,具有影响临床实践的潜力,特别是在全球范围内无法获得广泛的基因诊断和 MRI 的情况下。
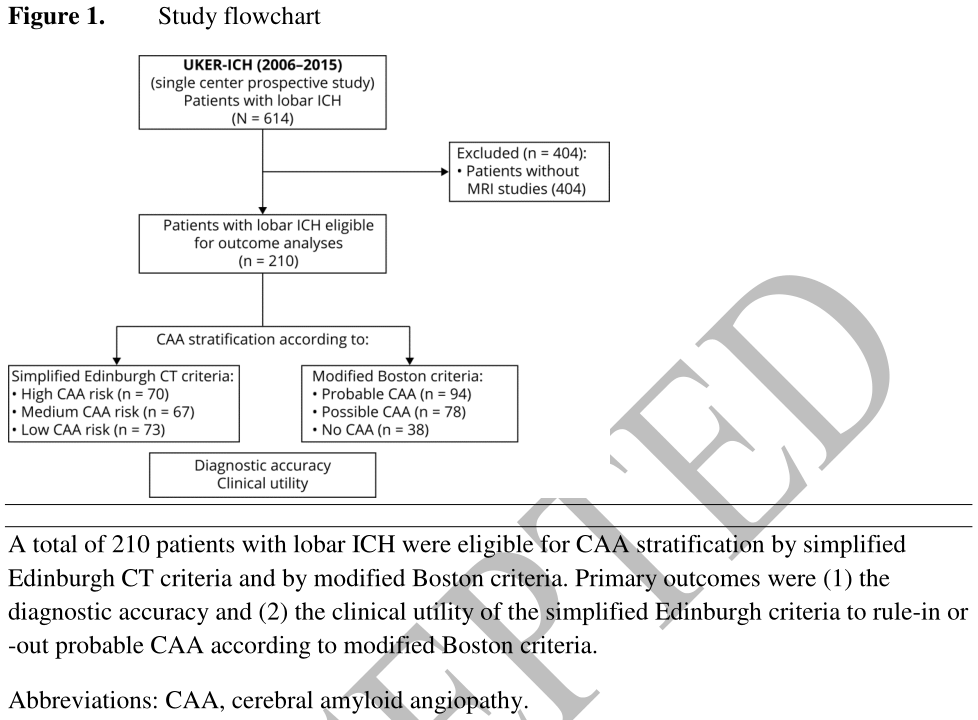
近日,有研究人员调查了简化的爱丁堡 CT 标准在识别潜在的脑淀粉样血管病 (CAA) 方面的准确性和临床实用性。本研究分析了(1)诊断准确性和(2)简化的爱丁堡CT诊断与CAA相关的大叶出血标准的临床应用价值,采用以MRI为基础的改良 Boston 标准作为独立参考标准。
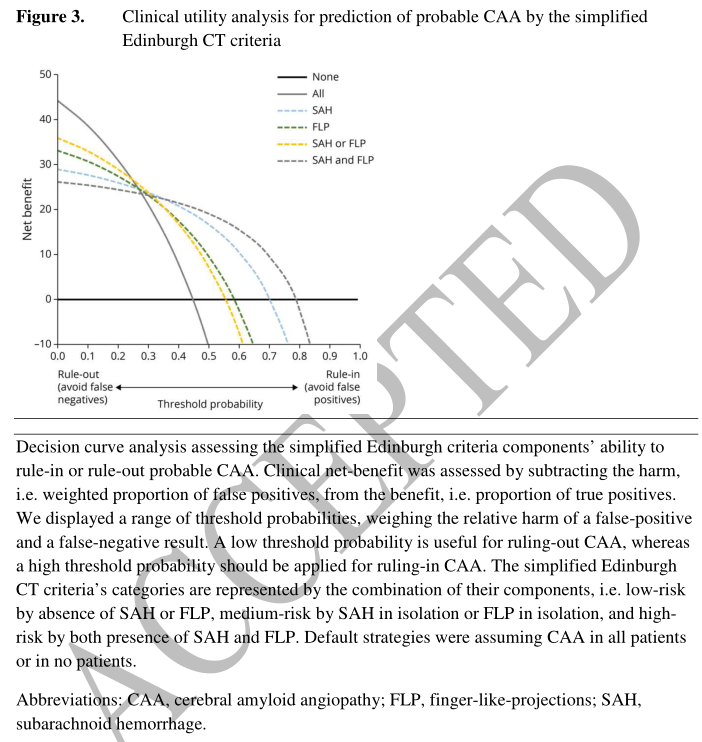
该外部验证分析了来自前瞻性单中心观察性队列研究(2006-2015,UKER-ICH,NCT03183167)。研究根据基于 MRI 的改良波士顿标准作为参考标准,调查了简化的基于爱丁堡 CT 标准的评估者间变异性和诊断准确性,以识别与可能的 CAA 相关的 ICH。通过决策曲线分析评估了简化的爱丁堡标准的效用,比较了高危类别(手指样投射和蛛网膜下腔出血)的理论临床净收益(不同阈值概率下的加权收益-危害),用于裁定和 低风险类别(既不是手指状突起也不是蛛网膜下腔出血)用于排除假设没有或所有患者患有 CAA(默认策略)。
- 根据爱丁堡 ct 简化标准,70例(33.3%)为高危型,67例(31.9%)为中危型,73例(34.8%)为低危型,表现为中等程度的评分差异。
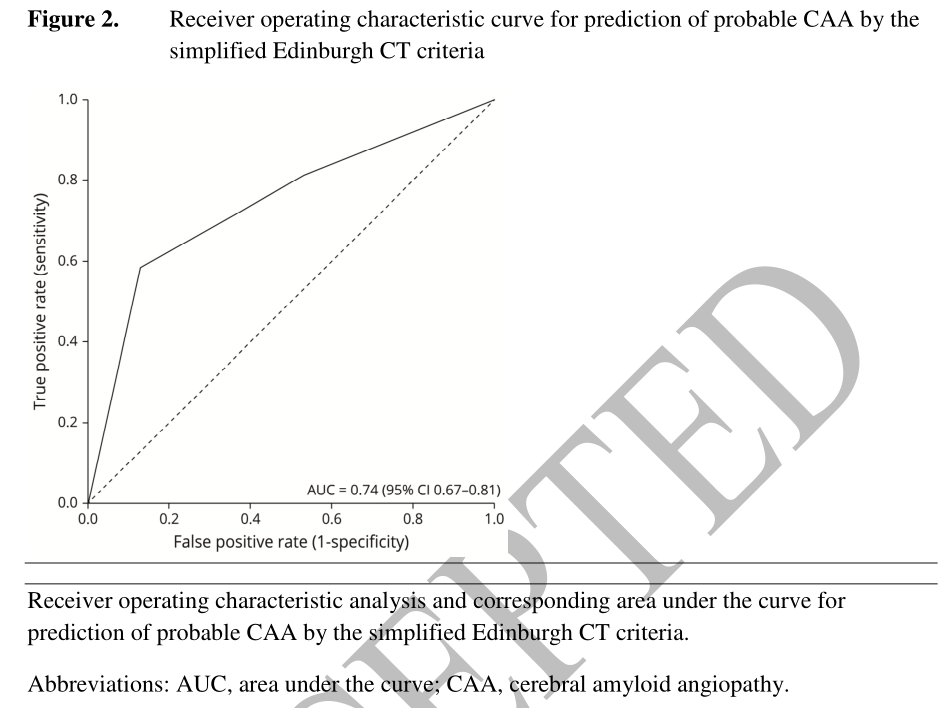
- 辨别力很好 (AUROC:0.74,95%CI 0.67–0.81),没有证据表明用于验证可能的 CAA 的基于 MRI 的诊断 (n=94/210,44.8%)校准不佳 (HosmerLemeshow,p=0.54)。
- 纳入标准即高风险的特异性为87.1%(79.3-92.3),排除标准即低风险的敏感性为80.9%(71.1-88.0)。
- 决策曲线分析表明,与默认策略相比,排除可能的 CAA 有理论上的临床净收益,但不能排除可能的 CAA。
应用简化的爱丁堡CT标准在诊断工作似乎临床上有用,可以准确地识别CAA患者的 lobar 脑出血。
这项研究提供了Ⅱ类证据,在大出血患者中,简化的爱丁堡标准准确地识别了那些高风险的CAA。
文献来源:
Sembill JA, Knott M, Xu M, et al. Simplified Edinburgh CT Criteria for Identification of Lobar Intracerebral Hemorrhage Associated With Cerebral Amyloid Angiopathy [published online ahead of print, 2022 Mar 21]. Neurology. 2022;10.1212/WNL.0000000000200261. doi:10.1212/WNL.0000000000200261
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#血管病#
41
#脑淀粉样#
43
简化爱丁堡CT标准比较实用
24
认真学习中!
32
#Neurol#
34
#脑淀粉样血管病#
46