The Lancet:核出口抑制剂XPOVIO显著延长复发或难治性多发性骨髓瘤患者的无进展生存期
2020-11-16 MedSci原创 MedSci原创
SVd治疗方案相比于Vd将PFS中位数增加了4.47个月(47%)。
柳叶刀(The Lancet)杂志于11月14日发表了多中心3期随机临床研究BOSTON的结果(NCT03110562),该研究共涉及402名复发或难治性多发性骨髓瘤成年患者,这些患者先前接受过一到三次治疗。这项研究旨在评估每周一次口服核出口选择性抑制剂XPOVIO(selinexor)联合每周一次的Velcade(硼替佐米)加低剂量地塞米松(SVd)与标准疗法(每周两次的Velcade+小剂量地塞米松,Vd)相比的疗效和安全性。研究主要终点是无进展生存期(PFS),主要次要终点包括总体缓解率(ORR)和周围神经病变率等。

研究结果显示:SVd组中位PFS为13.93个月,而Vd组为9.46个月,说明SVd治疗方案相比于Vd将PFS中位数增加了4.47个月(47%)。
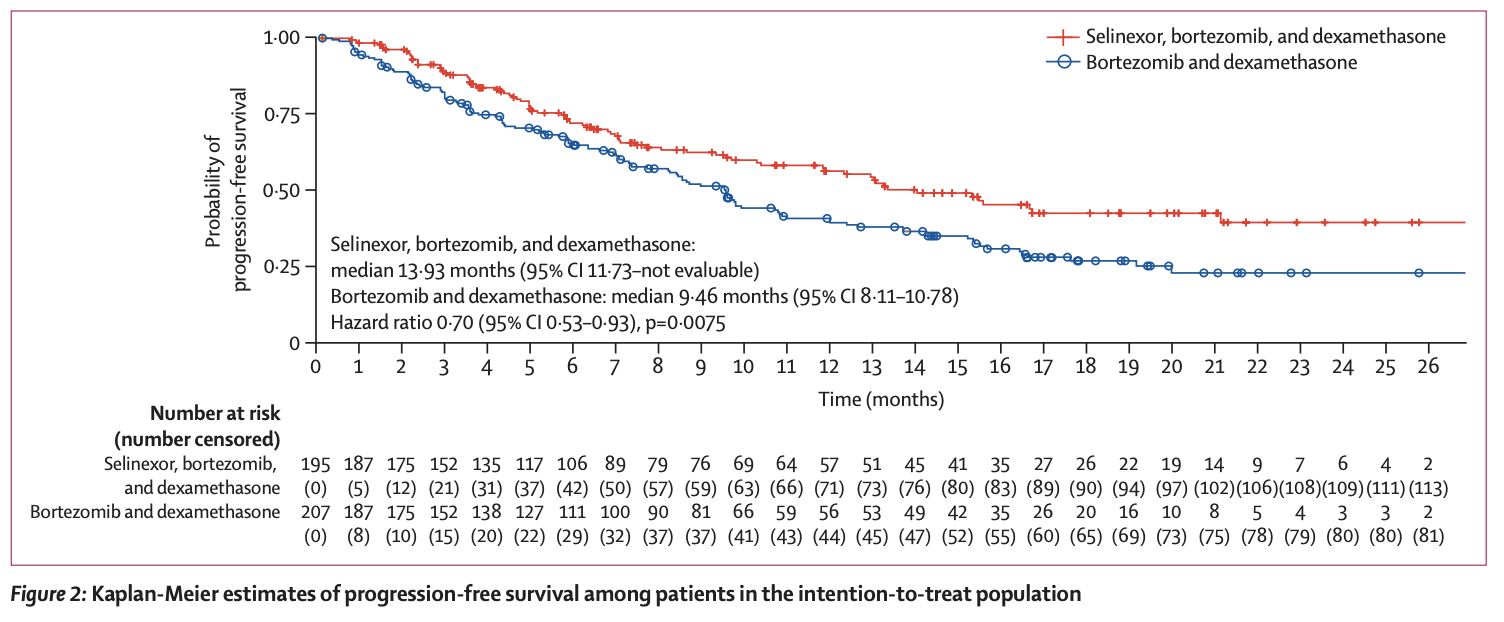
与Vd组相比,SVd组还显示出显着更高的ORR,分别为62.3%和76.4%,p = 0.0012。与Vd组相比,仅接受先前一种疗法的患者在SVd组的ORR也更高,分别为65.7%和80.8%,p = 0.0082。更重要的是,与Vd相比,SVd在几个重要的亚组中均显示出一致的PFS延长和更高的ORR。
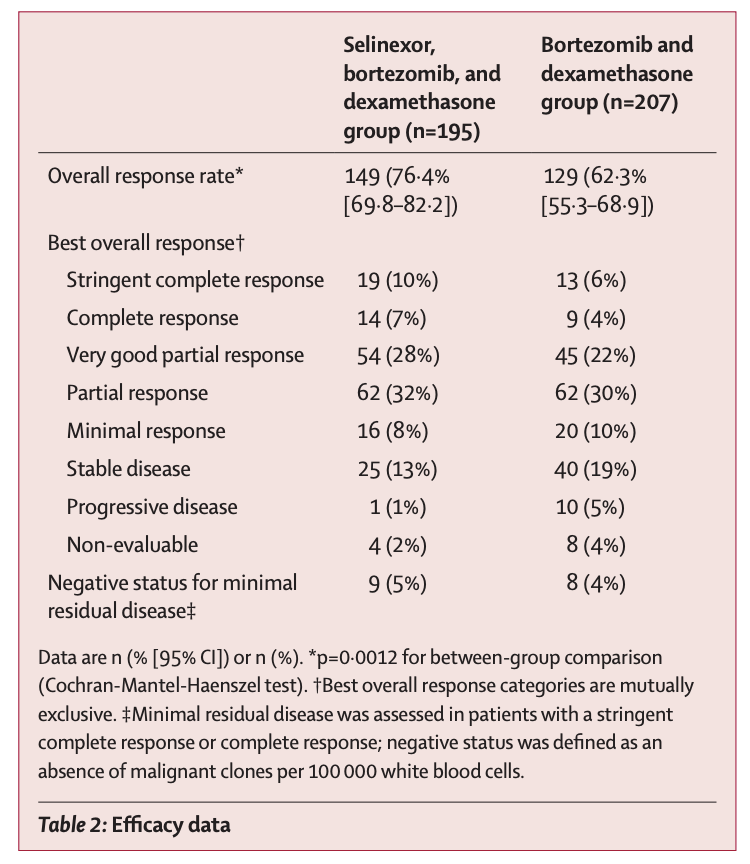
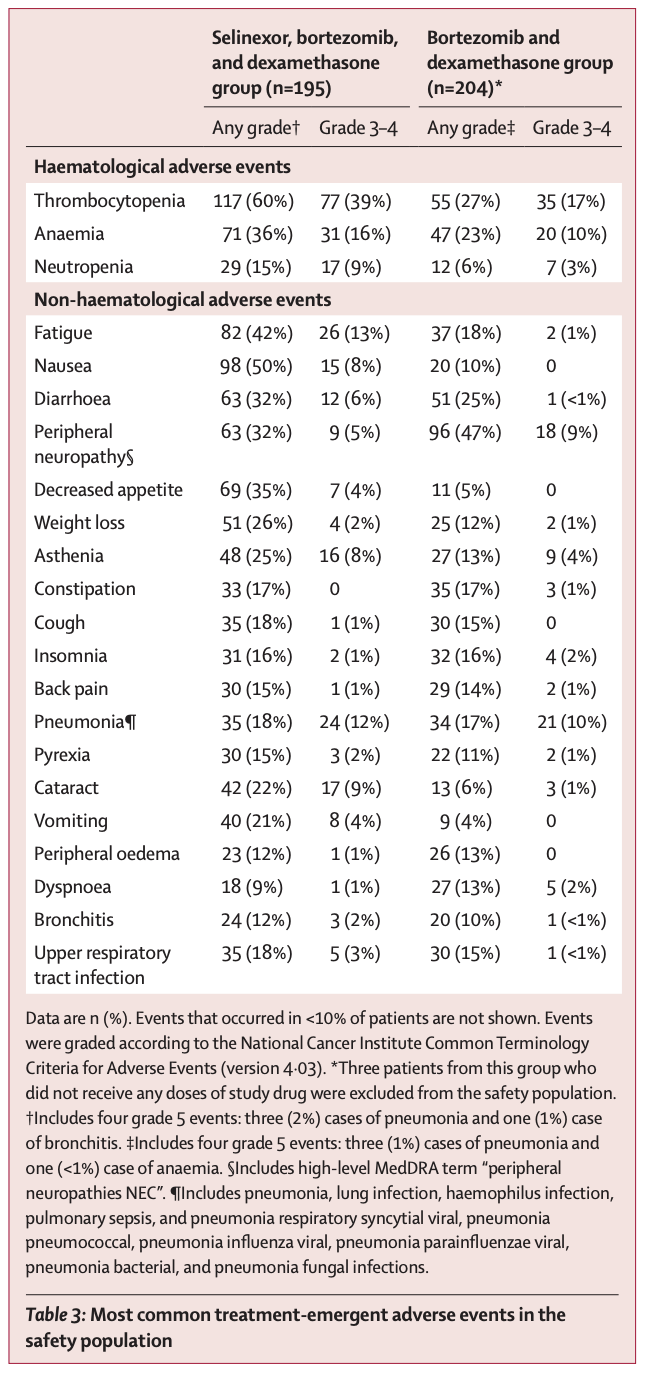
与Vd相比,SVd的周围神经病变(PN)率也显着降低,分别为32.3%和47.1%,p = 0.0010。SVd组≥2级PN率也比Vd组显着降低,分别为21.0%和34.3%,P = 0.0013。
最常见的紧急不良事件(AEs)为血细胞减少症和胃肠道症状,与先前其他selinexor研究报道的结果一致。大多数不良事件可通过调整剂量或标准支持治疗来控制。与血液学治疗相关的最常见不良事件是恶心(50%),疲劳(42%),食欲下降(35%)和腹泻(32%),主要是1级和2级事件。与治疗相关最常见的3级和4级AE是血小板减少症(39%),贫血(16%)和疲劳(13%)。
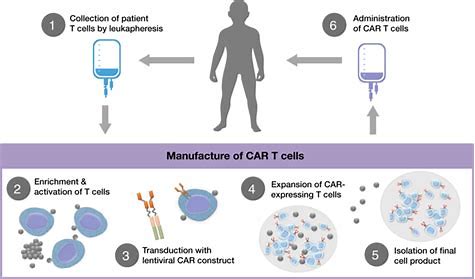
XPOVIO作为一线治疗用的口服核出口(SINE)选择性抑制剂,通过选择性结合并抑制核输出蛋白1(XPO1,也称为CRM1)发挥功能。XPOVIO通过阻断肿瘤抑制因子、生长调节蛋白和抗炎蛋白的核输出,引起这些蛋白在细胞核中积累发挥抗癌作用。
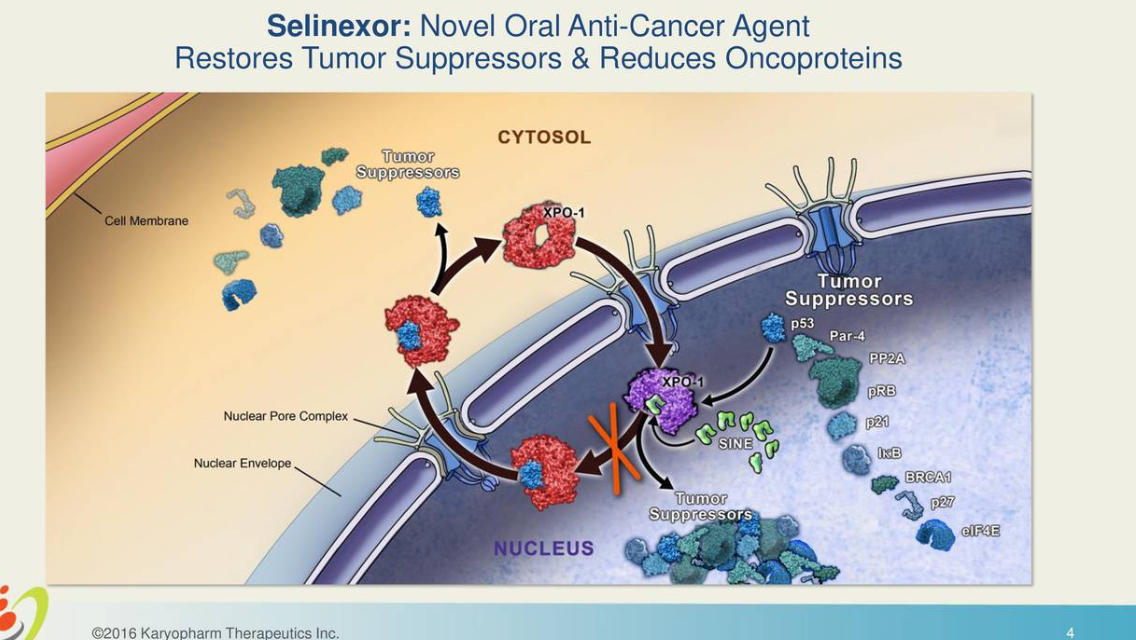
图片来源:https://seekingalpha.com/article/4058161-karyopharms-selinexor-should-drive-substantial-growth
原始出处:
Once-per-week selinexor, bortezomib, and dexamethasone versus twice-per-week bortezomib and dexamethasone in patients with multiple myeloma (BOSTON): a randomised, open-label, phase 3 trial. N Engl J Med. November 14, 2020 DOI:https://doi.org/10.1016/S0140-6736(20)32292-3
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Xpovio#
45
#多发性#
34
#Lancet#
23
#抑制剂#
24
#生存期#
31
#无进展生存期#
28
#难治性#
22
顶刊就是不一样,质量很高,内容精彩!学到很多
50