几十年来,皮肤黑色素瘤的发病率一直在稳步上升,从1950年代的1例/10万人增加到今天的30-50例/10万人,而且在初诊时肿瘤厚度达到1mm的薄黑色素瘤的概率也越来越高。这种增加主要是因为紫外线照射。
首个采用免疫检查点抑制剂辅助治疗II期黑色素瘤的随机试验的结果显示,肿瘤复发风险显著降低。该研究旨在评估两个独立的数据集,以进一步明确I-II期黑色素瘤患者的生存率。
德国的CMMR研究评估了2000年-2015年期间接受治疗的17544例I-II期原发性黑色素瘤患者。探索性队列纳入了6725位患者,验证队列纳入了10819位患者。主要终点是生存预后,与已报道的美国癌症联合委员会第8版(AJCCv8)I-II期患者的生存数据进行比较。
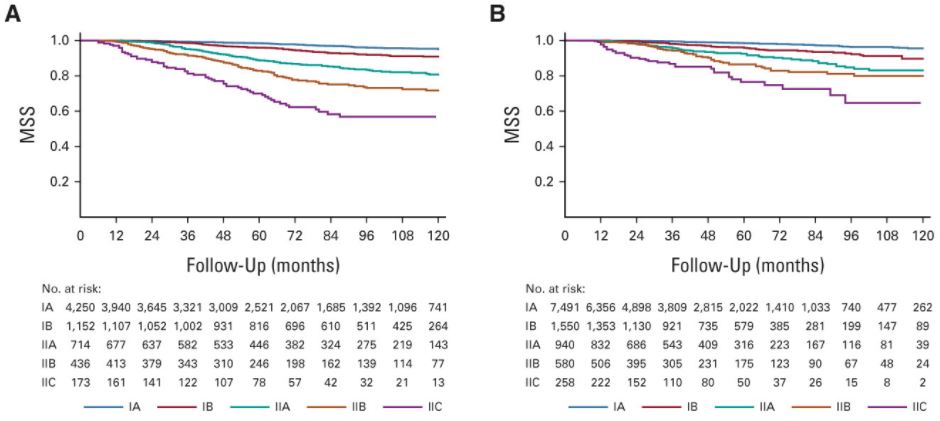
探索性队列(A)和验证性队列(B)的黑色素瘤特异性生存率
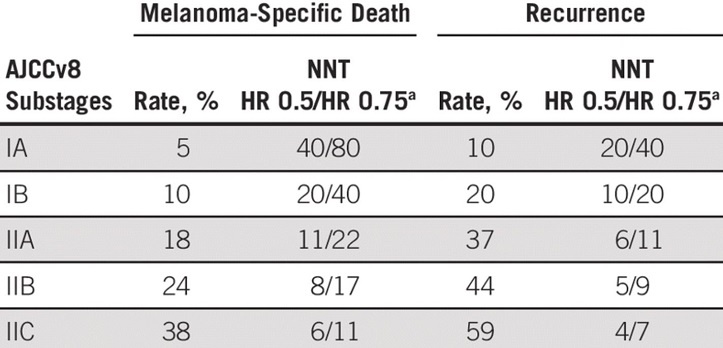
与AJCCv8队列相比,CMMR研究两个队列的IA期患者的10年黑色素瘤特异性生存率是:95.1%-95.6% vs 98%;CMMR研究队列和AJCCv8队列IB期患者的10年黑色素瘤特异性生存率为:89.7%-90.9% vs 94%;IIA期患者:80.7%-83.1% vs 88%;IIB期患者:72.0%-79.9% vs 82%;IIC期患者:57.6%-64.7% vs 75%。IA-IIA期患者的复发率大约是黑色素瘤特异性死亡率的两倍。
CMMR研究的黑色素瘤特异性死亡率和复发率
综上,在CMMR研究的两个队列中,I-II期黑色素瘤患者的黑色素瘤特异性生存率均逊色于已发表的AJCCv8队列结果。因此,这类患者或需要进行适当的辅助治疗。
原始出处:
Claus Garbe, et al. Prognosis of Patients With Primary Melanoma Stage I and II According to American Joint Committee on Cancer Version 8 Validated in Two Independent Cohorts: Implications for Adjuvant Treatment. Journal of Clinical Oncology. June 16, 2022. https://ascopubs.org/doi/full/10.1200/JCO.22.00202.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Oncol#
43
#色素#
42
#黑色素#
34
#黑色素#
39