Front Oncol:吡咯替尼VS T-DM1用于转移性HER-2阳性经治乳腺癌患者的疗效和安全性:来自贝叶网状Meta分析
2021-09-18 yd2015 MedSci原创
研究提示,吡咯替尼较T-DM1治疗转移性HER-2阳性经治乳腺癌患者更有效,但是发生≥3级不良事件也较高。
抗HER2治疗药物问世之前,HER2阳性乳腺癌患者的预后较差。第一个抗HER2药物曲妥珠单抗的临床应用,HER2阳性乳腺癌患者的预后得到明显改善。目前相继有帕妥珠单抗、T-DM1、拉帕替尼、吡格替尼等药物出现,改变了HER2阳性晚期乳腺癌患者的治疗格局和预后。但是对于一线曲妥珠单抗进展后,二线治疗的最佳方案没有明确。因此,我国研究学者开展了贝叶网状Meta分析,比较吡咯替尼对比T-DM1用于转移性HER-2阳性经治乳腺癌患者的疗效和安全性。相关结果发表在Frontiers in Oncology杂志上,研究表明吡咯替尼较T-DM1效果更好,但是也伴随更多≥3 级不良事件发生。

研究搜索PubMed, EMBASE,和Web of Science 数据库,截止2020年8月。纳入了比较不同抗HER2方案在转移性HER2阳性(≤二线治疗)既往曲妥珠单抗(Tra)和紫杉烷治疗进展乳腺癌患者疗效和安全性的随机临床研究。基于贝叶斯理论使用固定效应模式网络meta分析无进展生存期(PFS)、总生存期(OS)、总缓解率(ORR)和3级不良事件(AEs)。
研究最终纳入12项研究共4353例患者。9种治疗策略(T-DM1, Lap-Cap(拉帕替尼-卡培他滨), Tra-Cap(曲妥珠单抗-卡培他滨), Cap(卡培他滨), Ner(来那替尼), per - trac –Cap(帕妥珠单抗-曲妥珠单抗-卡培他滨), Pyr-Cap(吡格替尼-卡培他滨), atezolizumab (Ate)-T-DM1(阿替丽珠单抗-T-DM1)和Ner-Cap(来那替尼-卡培他滨))进行网状meta分析。在所有方案中,Lap- Cap和trac -Cap在试验数量和随机参与者数量上排名前两位。
12项研究均报道了无进展生存期(PFS)结果。对于无进展生存期(PFS),Pyr-Cap优于其他方案:T-DM1 (HR=0.77, 95%CI 0.70–0.86), Lap-Cap (HR=0.64, 95%CI 0.59–0.69), Tra-Cap (HR=0.63, 95%CI 0.56–0.70), Cap (HR=0.50, 95%CI 0.45–0.56), Ner (HR=0.59, 95%CI 0.51–0.69), Per-Tra-Cap (HR=0.68, 95%CI 0.59–0.79), 和Ner-Cap(HR=0.72, 95%CI 0.64–0.81)。根据SUCRA(99.4%)和MeanRank(1.1)的结果,Pyr-Cap可能时最好的治疗策略,其次是Ate-T-DM1(84.6%, 2.2)、T-DM1(75.0%, 3.0)、Ner-Cap(61.5%, 4.1)、Per-Tra- Cap(50.7%, 4.9)、Lap-Cap(34.3%, 6.3)、Tra-Cap(26.5%, 6.9)、Ner(17.9%, 7.6)和Cap(0.2%, 9.0)。

不同方案PFS对比
10项研究均报道了总生存期(OS)结果。对于总生存期(OS),Pyr-Cap优于Lap-Cap (HR=0.71, 95%CI 0.52–0.99), Cap (HR=0.68, 95%CI 0.49–0.96), 和Ner (HR=0.65, 95%CI 0.45–0.94)。Pyr-Cap 效果最好,而Ner 最差。
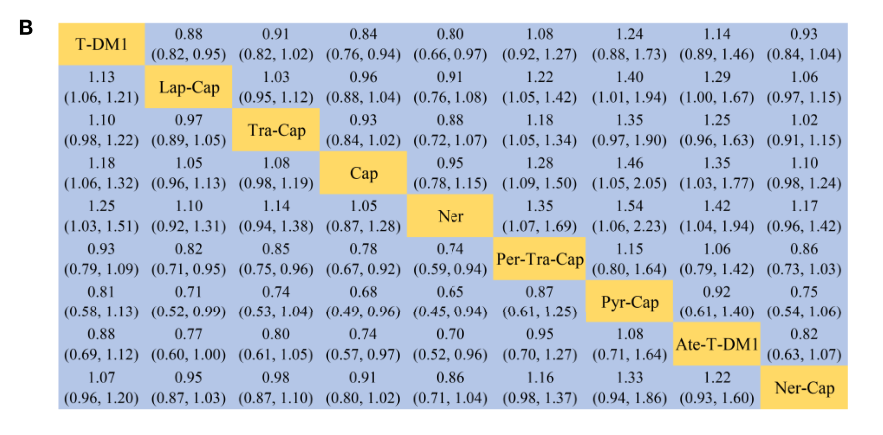
不同方案OS对比
10项研究均报道了ORR结果。对于ORR,Pyr-Cap优于Cap (ORR=7.87, 95%CI 1.22–56.51)。同样,对于ORR,Pyr-Cap效果最好,而Ner 最差。
治疗策略之间≥3级不良事件没有统计学差异。但是根据等级概率图,Pyr-Cap是发生≥3级AEs发生率最高的方案,而T-DM1是最低的方案。
综上,研究提示,吡咯替尼较T-DM1治疗转移性HER-2阳性经治乳腺癌患者更有效,但是发生≥3级不良事件也较高。
原始出处:
Liao H, Huang W, Liu Y, Pei W, Li H. Efficacy and Safety of Pyrotinib Versus T-DM1 in HER2+ Metastatic Breast Cancer Patients Pre-Treated With Trastuzumab and a Taxane: A Bayesian Network Meta-Analysis. Front Oncol. 2021 May 3;11:608781. doi: 10.3389/fonc.2021.608781. PMID: 34012912; PMCID: PMC8127838.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#疗效和安全性#
32
#Meta#
29
#Oncol#
35
#MET#
24
#转移性#
38
#HER-2#
29
#乳腺癌患者#
35
谢谢梅斯分享这么多精彩信息
57
HER2药物曲妥珠单抗的临床应用,HER2阳性乳腺癌患者的预后得到明显改善。
57