ROBINS-I量表:非随机对照试验研究偏倚风险评价
2019-01-29 MedSci整理 MedSci整理
偏倚风险(risk of bias)评价是系统评价/Meta分析制作中不可或缺的重要环节,其意义在于针对某个问题,偏倚是否是"可接受的"。它不仅能部分反应纳入文献的“质量”,也是系统评价/Meta分析证据级别的间接反映指标。在众多观察性研究偏倚风险评价量表中,ROBINS-I是最被方法学家认可的量表之一,Cochrane 手册将其推荐为观察性研究偏倚风险首选工具。 ROBINS-I量表分
偏倚风险(risk of bias)评价是系统评价/Meta分析制作中不可或缺的重要环节,其意义在于针对某个问题,偏倚是否是"可接受的"。它不仅能部分反应纳入文献的“质量”,也是系统评价/Meta分析证据级别的间接反映指标。在众多观察性研究偏倚风险评价量表中,ROBINS-I是最被方法学家认可的量表之一,Cochrane 手册将其推荐为观察性研究偏倚风险首选工具。
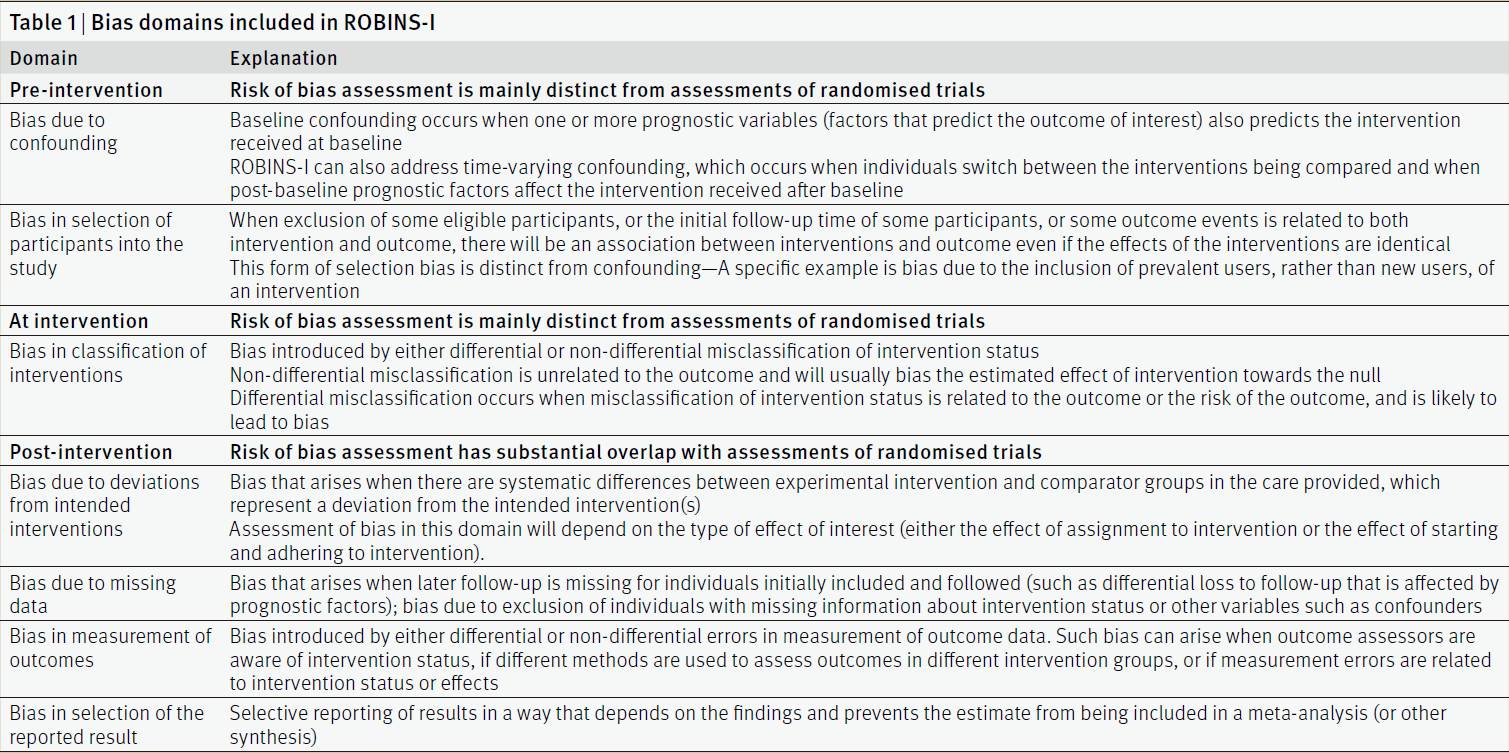
ROBINS-I量表分为7个域(domain),这7个域包括:混杂偏倚(bias due to confounding)、受试者/参与者选择偏倚(bias in selection of participants into the study)、干预/暴露分类偏倚(bias in classification of interventions)、暴露偏差偏倚(bias due to deviations from intended interventions)、数据缺失偏倚(bias due to missing data)、结局测量偏倚(bias in measurement of outcomes)和选择性报告偏倚(bias in selection of the reported result)。每个域里面又有若干条目组成。
相对于其他量表,ROBINS-I量表一个明显的优点是能较全面的反映纳入研究的偏倚风险。例如,ROBINS-I考虑了基本信息收集量表(questionnaire)的效度和信度,考虑了针对随访过程中随着时间变化而变化的时变混杂因素 (time-varying confounding),考虑了缺失值在各组中的平衡性和处理办法的可靠性,考虑了统计分析方法使用的合理性,以及考虑了结果是否存在选择性报告等问题。而这些常见问题在众多同类量表中很少被兼顾。当然ROBINS-I量表条目的理解及应用相对于其他量表稍微复杂。以下是ROBINS-I量表的完整介绍。
ROBINS-I曾经也叫做ACROBAT-NRSI (A CochraneRisk Of Bias Assessment Tool: for Non- Randomized Studies of Interventions),是改良了的非随机干预研究偏倚风险评估工具,由来自世界各地的研究者经过3年多的研究,于2016年发表在British Medical Journal(BMJ)杂志。
ROBINS-I与Cochrane的RCT偏倚风险评估工具相似,也有7个评价维度(domain),包括:Confounding(混杂偏倚), Selection bias(选择偏倚), Bias in measurement classification of interventions(干预措施分类偏倚), Bias due to deviationsfrom intended interventions(实施偏倚), Bias due to missing data(失访偏倚), Bias in measurement of outcomes(测量偏倚), Bias in selection of the reported result(报告偏倚)。对于Non-RCT的质量评价,因为是否随机分组对分组以后的bias没有影响,所以ROBINS-I不再关心是否随机分组和分配隐藏,而强调混杂偏倚,选择偏倚,干预措施分类偏倚,而其余4个维度则与Cochrane的RCT偏倚风险评估工具重叠,也就是测量偏倚、实施偏倚、失访偏倚、报告偏倚。(Table 1,取自BMJ原文)
其中,每一个维度都有一系列的问题,以Confounding为例,有8个问题,对每一个问题进行“Yes”,“Probably yes”,“Probably no”,“No”以及“No information”等的判断,最后综合判断这一维度的风险等级,包括“Low risk(低风险)”, “Moderate risk(中度风险)”, “Serious risk(严重风险)” and “Critical risk(致命风险)”。以此类推得出所有7个维度的风险等级。

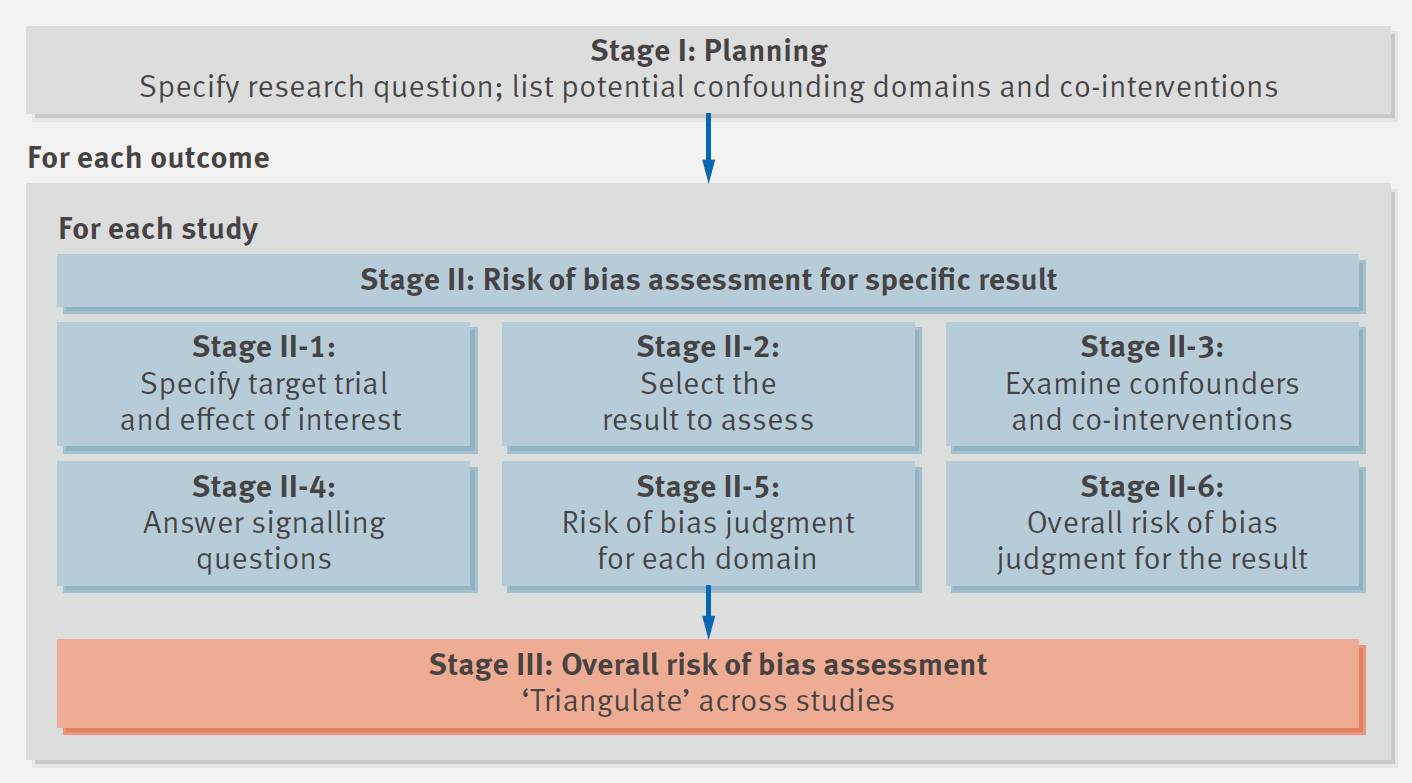
至于具体操作的时候,是先假想出一个“目标实验(Target trial)”,这个假想的目标实验不需要现实可行或者符合伦理要求,能够得出我们想要获得的结果的一个理想研究。将每个评价的研究看做这个目标实验的近似,然后根据每个维度里的提示问题(signalling questions),得出每个问题的答案,根据这些问题确定该维度的等级是low, moderate, serious, 或者critical。最终再根据每一个维度的风险等级,参考风险评价标准,综合判断一个研究的风险等级。具体流程见下图(图片取自BMJ原文)。
相比NOS,ROBINS-I要复杂的多,耗时也多。然而要评价非随机对照临床实验的偏倚风险,ROBINS-I应该是一个更合适的评价工具,特别是在未来的高质量的meta分析中,Non-RCT的偏倚风险评价用ROBINS-I是大势所趋。
内容来自徐畅、李玲、赵一鸣等
原始出处:
Sterne JAC,Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias innon-randomised studies of interventions. Bmj, 2016, 355
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











没错,ROBINS-I是大势所趋。
39
非常好的一篇对文献的概括和说明,受益匪浅。
62
#对照#
28
#风险评价#
33
#对照试验#
23
#随机对照试验#
25
#评价#
35