JACC Cardiovasc Interv:经桡动脉PCI抗凝:比伐卢定真的比肝素更出色?
2017-06-30 选题审校:顾歆纯 编辑:贾朝娟 环球医学
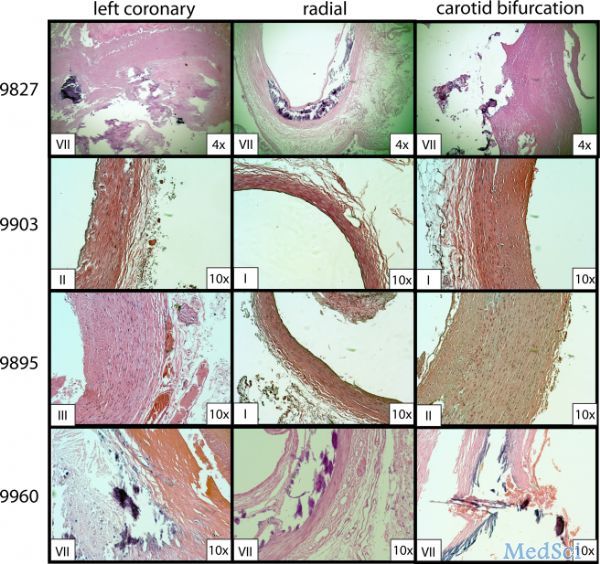
既往有研究显示,经桡动脉行经皮冠脉介入(PCI),比伐卢定抗凝优于肝素。但近期的研究并未显示这一优越性。2017年6月,发表在《JACC Cardiovasc Interv》的一项研究显示,比伐卢定或肝素抗凝的死亡、心肌梗塞或卒中的复合终点没有差异。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ASC#
30
#比伐卢定#
40
#经桡动脉#
32
#JACC#
33
#ACC#
28
#桡动脉#
25