Circulation:糖尿病心血管疾病患者的危险因素和预后的关系
2017-06-19 MedSci MedSci原创
改变一些危险因素可以显着改善伴有糖尿病的心血管患者的预后。但是,将这些危险因素改变到什么程度才能最大化改善预后仍没有大型的临床试验数据支持。
改变一些危险因素可以显著改善伴有糖尿病的心血管患者的预后。但是,将这些危险因素改变到什么程度才能最大化改善预后仍没有大型的临床试验数据支持。
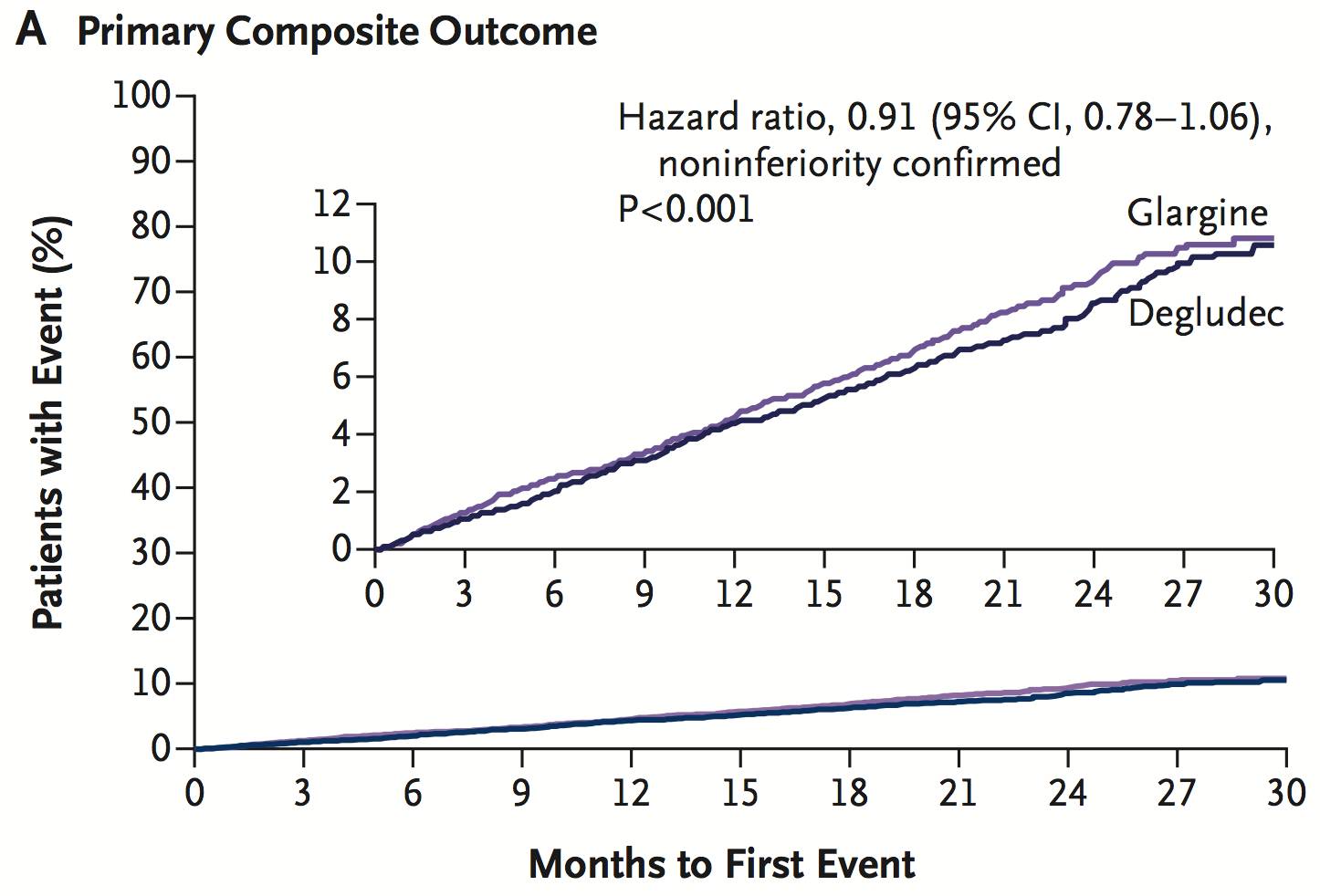
本研究通过对来自38个国家的13616例患有糖尿病和心血管疾病的患者在以下5个指标进行分析评估:阿司匹林的使用、脂质的控制(低密度脂蛋白胆固醇<70mg/dl或接受他订类药物治疗)、血压控制(收缩压<140mmHg,舒张压<90mmHg)、血管紧张素转换酶抑制剂或血管紧张素受体阻断剂的使用和无烟状态。利用Logistic回归评估个体与区域因素和二级预防成果的关系。利用Cox比例风险回归分析评估基线的二级预防成果与心源性死亡、心梗和卒中的关系。
研究结果显示,有71.8%的患者达到了其中的4个指标,而29.9%的患者达到了全部的5个指标。其中以北美的患者居多(41.2%),西欧、东欧和拉丁美洲约占25%。在个体因素中,血压控制(57.9%)达标率最低,而无烟状态(89%)的达标率最高。通过超过平均3年的随访时间,发现高的二级预防成果分数与良好的预后结局是相关的(HR:0.6[95% Cl:0.47-0.77]相对于这些达到5个指标和≤2个的患者来说)。
本次大型临床研究结果证实,通过改变危险因素是可以显著改善伴有糖尿病的心血管患者预后的。
原始出处:
Neha J. P et al.Secondary Prevention of Cardiovascular Disease in Patients with Type 2 Diabetes: International Insights from the TECOS Trial.Circluation.2017 June.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#疾病患者#
38
#糖尿病心血管#
31
学习了
82
#血管疾病#
41
学习了。。。。。
63