病例分享:在感染诊疗中,PCT的动态监测才是神助攻!
2017-12-09 佚名 梅里埃诊断
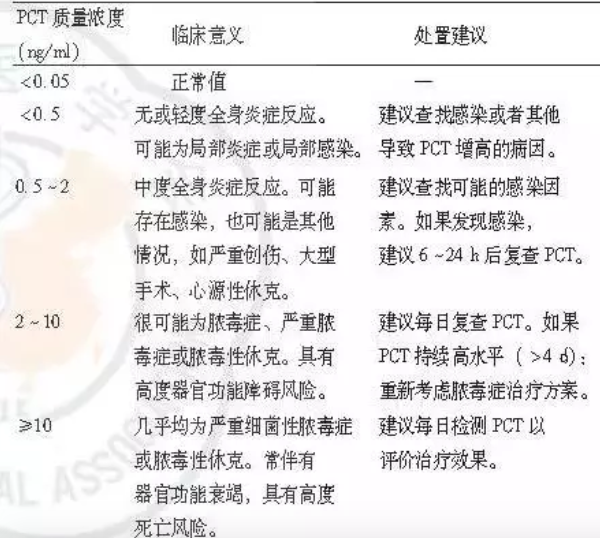
意大利曼图亚Carlo Poma医院ICU科室的GianPaolo CASTELLI医生,分享了一个PCT动态监测的病例,展示了PCT是如何通过诊断、预后、治疗和抗生素管理等在临床决策制定程序中提供附加值的。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PCT#
31
学习下.有了解过之前
58
学习了,很好
60
学习了.关注中
73
学习学习.了解了解
63
学习了受益匪浅
62
学习一下
19