Cell Res:季红斌发现新的肺鳞癌致病融合基因TRA2B-DNAH5
2016-09-29 MedSci MedSci原创
9月27日,国际学术期刊Cell Research在线发表了中国科学院上海生命科学研究院生物化学与细胞生物学研究所季红斌研究组的最新研究成果“Identification of TRA2B-DNAH5 fusion as a novel oncogenic driver in human lung squamous cell carcinoma”。该研究鉴定出人肺鳞癌中一个新的
9月27日,国际学术期刊Cell Research在线发表了中国科学院上海生命科学研究院生物化学与细胞生物学研究所季红斌研究组的最新研究成果“Identification of TRA2B-DNAH5 fusion as a novel oncogenic driver in human lung squamous cell carcinoma”。该研究鉴定出人肺鳞癌中一个新的致病融合基因TRA2B-DNAH5,并揭示了该致病基因的作用机制及潜在的治疗药物。
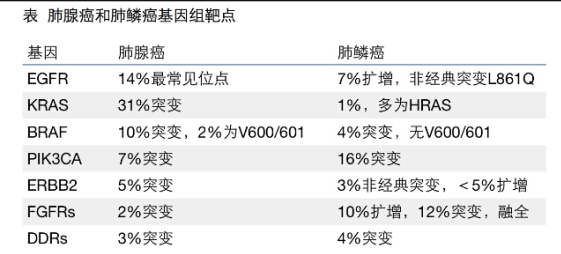
全球范围内肺癌的发病率和死亡率高居不下。 非小细胞肺癌约占所有肺癌的80%左右,主要包括肺腺癌和肺鳞癌。对于肺癌的治疗,与传统的放疗和化疗相比,分子靶向治疗是一种极具前景的治疗方法,而这项治疗技术的发展在极大程度上依赖于肺癌中致病基因的发现。随着基因组学和测序技术的发展,越来越多的致病基因被鉴定。目前肺腺癌中致病基因图谱已经比较清楚。季红斌研究组一直致力于肺癌致病基因的鉴定,在前期工作中揭示了约90%非吸烟人群来源的肺腺癌中的关键致病基因图谱,之前就通过外显子芯片分析的方法,成功地在肺腺癌中鉴定了RET融合基因(Cell Res 2012)并发明了一种用于检测RET融合基因的方法(ZL 2012 1 0069592.3)。相对而言,肺鳞癌致病基因的发现非常之少,这在很大程度上限制了肺鳞癌中分子靶向治疗的发展。
在该研究中李飞、方兆元和张箭在季红斌研究员的指导下,首先通过外显子芯片分析、5’RACE及测序的方法,在肺鳞癌样本中成功地鉴定一个新的驱动基因:TRA2B-DNAH5融合基因。研究人员通过RT-PCR的方法对163例肺鳞癌样本进行分析,发现其中5例 (3.1%)具有TRA2B-DNAH5融合基因。一系列功能研究结果表明,TRA2B-DNAH5融合基因是一个致病融合基因。机制研究发现TRA2B-DNAH5融合基因通过SIRT6-ERK1/2-MMP1 信号轴来促进肺鳞癌的恶性进展。裸鼠移植瘤模型的实验结果揭示MEK1/2抑制剂Selumetinib可以有效抑制TRA2B-DNAH5融合基因的肺鳞癌恶性进展。Selumetinib已经在黑色素瘤临床三期试验中。该研究提示Selumetinib有可能成为靶向治疗具有TRA2B-DNAH5融合基因的肺鳞癌患者的潜在药物,为临床上这类肺癌患者提供新的治疗方案。
李飞、方兆元和张箭为该论文的共同第一作者,季红斌研究员为通讯作者。该工作得到了复旦大学肿瘤医院陈海泉教授、孙艺华副教授,生化与细胞所曾嵘研究员、李辰副研究员、哈佛大学医学院魏文毅副教授以及生化与细胞所分子生物学技术平台、细胞分析技术平台以及动物实验技术平台的大力支持。该工作得到国家自然科学基金委员会、上海市科学技术委员会、中国博后基金、上海市博后基金及中国科学院的经费支持。(生化与细胞所)

图示:(A) 65例肺鳞癌样本和配对的5例正常肺样本外显子芯片热图显示207LC样本具有潜在的DNAH5基因融合,箭头指示潜在基因融合位点。(B) TRA2B的N端12个氨基酸与DNAH5的C端的3823个氨基酸融合形成一个新的TRA2B-DNAH5融合蛋白。
原始出处:
Li F, Fang Z, Zhang J, Li C, Liu H, Xia J, Zhu H, Guo C, Qin Z, Li F, Han X, Wang Y, Feng Y, Wang Y, Zhang W, Wang Z, Jin Y, Sun Y, Wei W, Zeng R, Chen H, Ji H. Identification of TRA2B-DNAH5 fusion as a novel oncogenic driver in human lung squamous cell carcinoma. Cell Res. 2016 Sep 27. doi: 10.1038/cr.2016.111
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Cell#
31
#TRA#
21
参考学习,继续关注
60
#CEL#
24
文章很好,继续关注
73
继续关注
63
继续学习
2
#肺鳞癌#
34
#鳞癌#
31
#融合#
18