J Hypertens:长期血压变异性预测心血管风险的效能分析
2018-09-20 xing.T MedSci原创
由此可见,BP变异性与CVD之间的关联在大型数据集中具有统计学意义,但并未显著改善心血管风险评分的性能。
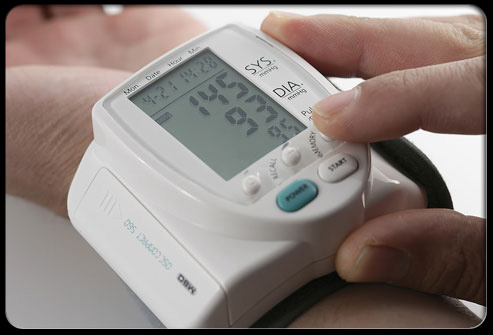
血压(BP)是心血管疾病(CVD)的长期危险因素。SBP广泛应用于临床决策的心血管风险评分。最近,个体BP变异性已被证明是CVD的主要预测指标。高血压领域权威杂志Journal of Hypertension上发表了一篇研究文章,研究人员旨在明确将BP变异性与标准危险因素相结合是否可以改善心血管危险评分。
研究人员使用2005年1月1日年龄为40-74岁患者的队列数据,这些患者来自临床实践研究Datalink,这是一个源自电子健康记录的研究数据库。研究人员将医院事件和死亡率数据相关联。在多达六次门诊就诊时测得的血压计算出与平均值无关的SBP变异性。研究人员将数据在地理上划分为派生和验证数据集。在派生数据集中,研究人员开发了一个参考模型,其中包含了先前评分中使用的危险因素和指数模型,其中包含相同的因子和BP变异性研究人员在包含可校准比率和c统计量的验证数据集中计算了模型验证统计数据。
在派生数据集中,BP变异性与CVD相关,并与其它危险因素无关(P=0.005)。然而,在验证数据集中,两个模型具有相似的c统计量(分别为0.7415和0.7419)、R2(分别为31.8和32.0)和校准比率(分别为0.938和0.940)。
由此可见,BP变异性与CVD之间的关联在大型数据集中具有统计学意义,但并未显著改善心血管风险评分的性能。
原始出处:
Stevens, Sarah L.et al. The utility of long-term blood pressure variability for cardiovascular risk prediction in primary care. Journal of Hypertension. 2018. https://journals.lww.com/jhypertension/Abstract/publishahead/The_utility_of_long_term_blood_pressure.97346.aspx
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#TENS#
33
#血管风险#
39
#PE#
34
#能分析#
44
#变异#
32
#血压变异性#相信未来5年是热点,不仅关心血压高与低,还要关注血压变异性才可以
47