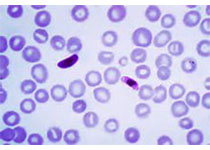
Blood:树突细胞疫苗可以预防或延迟AML缓解期患者复发。
2017-08-23 qinqiyun MedSci原创
复发是急性髓性白血病(AML)的主要问题,严重影响患者的存活期。现有研究发现,电转WT1-mRNA的树突细胞疫苗可以在一定程度上预防或延缓AML缓解期患者复发急性白血病。
中心点:
WT1 mRNA电转的树突细胞可以预防或延迟43%的经化疗后进入缓解期的AML患者复发。
总体存活率比SALR的最新存活数据更高,与分子和WT1特异性CD8+T细胞反应相关。
摘要:
复发是急性髓性白血病(AML)的主要问题,严重影响患者的存活期。在一II期研究中,研究人员在30位高复发风险的AML患者中研究电转Wilms'肿瘤(WT1)mRNA的树突细胞(DCs)疫苗用于诱导缓解后治疗的效果。
13位患者出现抗白血病反应。9位患者获得分子水平的缓解,其中5位缓解期维持至随访中位时间109.4个月后。另外4位患者获得疾病稳定。
有反应者的5年整体存活率(OS)比无反应者的要高(53.8% 比 25.0%;p=0.01)。在首次缓解期(CR1)接受DCs的患者中,复发率下降25%,有反应者的5年无复发生存期高于无反应者的(50% 比7.7%;p<0.0001)。在CR1接受DCs的≤65岁和>65岁两个分层的患者中,5年整体存活率分别是69.2%和30.8%(瑞典急性白血病注册[SALR]分别是51.7%和18%)。长期临床反应与循环中多抗原表位的WT1特异性CD8+T细胞的频数相关。长期总体存活率与迟发型高敏反应CD8+T淋巴细胞的干扰素-γ+和肿瘤坏死因子-α+WT1特异性反应相关。
总而言之,标准化疗后进入缓解期的AML患者接种电转WT1-mRNA的DCs疫苗是预防或延迟复发的有效措施,可提高患者的总体存活率。
原始出处:
Sebastien Anguille,et al.Dendritic cell vaccination as post-remission treatment to prevent or delay relapse in acute myeloid leukemia.Blood.August 22,2017.https://doi.org/10.1182/blood-2017-04-780155
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#缓解期#
36
#树突细胞#
45
学习了受益匪浅.
57