JCI:ADAM28介导乳腺癌转移
2012-06-17 Beyond 生物谷
ADAM28属于ADAM基因家族的金属蛋白酶,能切割血管性血友病因子(vWF)和抑制VWF介导肿瘤细胞凋亡,从而提高肺转移,假如抑制其表达的话能大幅减少肺转移,最新研究成果发表在Journal of The National Cancer Institute杂志上。 ADAMs与肿瘤的生长发展联系在一起,ADAM28在乳腺癌和非小细胞肺癌中过度表达,但ADAM28介导转移的机制是未知的。 为了
ADAM28属于ADAM基因家族的金属蛋白酶,能切割血管性血友病因子(vWF)和抑制VWF介导肿瘤细胞凋亡,从而提高肺转移,假如抑制其表达的话能大幅减少肺转移,最新研究成果发表在Journal of The National Cancer Institute杂志上。
ADAMs与肿瘤的生长发展联系在一起,ADAM28在乳腺癌和非小细胞肺癌中过度表达,但ADAM28介导转移的机制是未知的。
为了弄清ADAM28的作用,Satsuki Mochizuki博士和同事筛选了ADAM28可能影响的蛋白,发现VWF是其主要作用的蛋白。ADAM28影响VWF诱导的细胞凋亡作用,在小鼠模型研究中发现其抑制后,人肺癌和乳腺癌细胞的肺转移能力减小。
研究人员发现抑制ADAM28的表达或活性能使得肺转移大幅减少,血管中肿瘤细胞凋亡增加。在这项研究中,研究数据表明VWF诱导许多人细胞癌、肺癌、乳腺癌等肿瘤细胞凋亡,但只有当这些肿瘤细胞低表达ADAM28后,上述现象才出现。研究人员指出该研究的局限性在于该模型不能模拟出自发的人类癌症转移的过程,但结果表明ADAM28有促进癌细胞增殖和自发转移到远处器官的双向作用

doi:10.1093/jnci/djs232
PMC:
PMID:
Effect of ADAM28 on Carcinoma Cell Metastasis by Cleavage of von Willebrand Factor
Satsuki Mochizuki, Kenji Soejima, Masayuki Shimoda, Hitoshi Abe, Aya Sasaki, Hirotaka James Okano, Hideyuki Okano and Yasunori Okada
Background A disintegrin and metalloproteinase 28 (ADAM28) is implicated in tumor growth and metastasis in human breast and non–small cell lung carcinomas. We explored the mechanism of ADAM28-mediated metastasis by searching for new substrates of ADAM28.
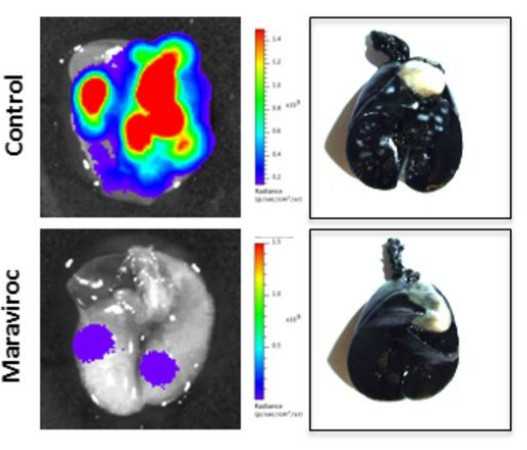
Methods We used a yeast two-hybrid system to screen the human lung cDNA library for ADAM28-binding proteins and identified von Willebrand factor (VWF) as a potential candidate. Binding was confirmed using yeast two-hybrid and protein binding assays, and ADAM28-mediated cleavage of VWF was analyzed by immunoblotting. Exogenous VWF-induced apoptosis in vitro was examined in human lung carcinoma (PC-9 and Calu-3), breast carcinoma (MDA-MB231 and MCF-7), renal cell carcinoma (Caki-2 and 769P), and hepatocellular carcinoma (HepG2) cells, and expression of ADAM28 was assessed by reverse transcription–polymerase chain reaction and immunoblotting. Effect on lung metastasis of PC-9 and MDA-MB231 cells was assessed by knockdown of ADAM28 expression using short hairpin RNAs (ADAM28-shRNA) and small interfering RNAs (ADAM28-siRNA), and inhibition of activity using neutralizing anti-ADAM28 antibody, in a mouse xenograft model by in vivo imaging (n = 9 mice per group). All statistical tests were two-sided.
Results ADAM28 could bind to and cleave native VWF. Cells with very low ADAM28 expression (MCF-7, 769P, and HepG2) were susceptible to VWF-induced apoptosis, whereas cells with high expression (PC-9, Calu-3, MDA-MB231, and Caki-2) were resistant. Knockdown of ADAM28 expression in PC-9 and MDA-MB231 cells by shRNA showed increased carcinoma cell apoptosis mainly in lung blood vessels and statistically significantly decreased lung metastasis at week 3 after injection (PC-9-control [n = 9 mice] vs PC-9-ADAM28-shRNA [n = 9 mice]: mean count = 198 × 106 vs 37 × 106 photons/s, difference = 161 × 106 photons/s, 95% confidence interval = 134 × 106 to 188 × 106 photons/s, P < .001). Similar inhibition of lung metastasis was observed with ADAM28-siRNA and anti-ADAM28 antibody.
Conclusion ADAM28 cleaves and inactivates proapoptotic VWF in carcinoma cells and enhances lung metastasis probably by promoting carcinoma cell survival within the blood vessels.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JCI#
29
#ADA#
22
#癌转移#
34