ASCO 2021:中国之声!特瑞普利单抗一线治疗复发/转移性鼻咽癌研究取得突破性进展,有望改写国际新标准!
2021-06-07 rayms 梅斯医学
值得关注!
2021年6月7日,2021年ASCO(美国临床肿瘤学会)年会以全体大会“重磅研究摘要”(LBA,Late-breaking Abstract)形式,发布了一项君实生物自主研发的抗PD-1单抗药物特瑞普利单抗联合化疗一线治疗复发/转移性鼻咽癌研究(JUPITER-02研究)最新成果。这是自ASCO年会有线上官方记录以来,首个入选全体大会的中国本土创新药物研究。

鼻咽癌是一种发生于鼻咽部黏膜上皮的恶性肿瘤,是常见的头颈部恶性肿瘤之一。据世界卫生组织统计,2020年在全球范围内确诊的鼻咽癌新发病例数超过13万,其中近半数发生在中国。中国南方(如广东、广西)和东南亚地区尤其高发。我国数据显示,中国I期到IV期的鼻咽癌患者平均5年生存率已达80%以上,处于国际较高水平。但在临床实践中,复发/转移性鼻咽癌给患者带来巨大痛苦。
目前,治疗手段有限,约10%的鼻咽癌患者经调强放疗(IMRT)±化疗后出现局部、区域复发,4%-10%初诊和15%-30%根治性治疗后鼻咽癌出现远处转移。对于复发或转移性鼻咽癌,一线标准治疗方案是以铂类为基础的两药联合化疗,但治疗后中位无进展生存时间仅有7个月左右,5年总体生存率小于20%,亟需由新的治疗方案来打破治疗瓶颈。
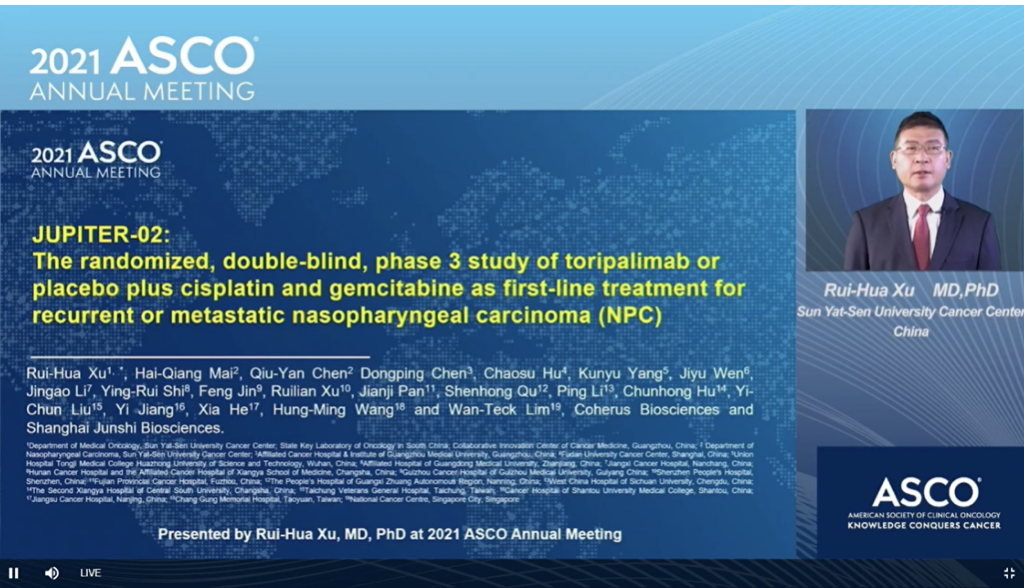
徐瑞华教授在ASCO年会全体大会上介绍JUPITER-02研究
此次入选的JUPITER-02研究(NCT03581786)是一项随机、双盲、安慰剂对照、全球多中心的III期试验,由中山大学肿瘤防治中心徐瑞华教授担任主要研究者,旨在比较特瑞普利单抗联合吉西他滨/顺铂与安慰剂联合吉西他滨/顺铂作为复发性或转移性鼻咽癌患者一线治疗方案的疗效和安全性。这也是迄今为止,全球范围内规模最大的免疫检查点抑制剂联合化疗一线治疗复发或转移性鼻咽癌的III期临床研究。
该研究在中国大陆、中国台湾、新加坡共纳入自2018年11月至2019年10月289例未接受过化疗的复发/转移性鼻咽癌患者,随机(1:1)分配患者至特瑞普利单抗(240mg, Q3W)联合化疗(吉西他滨和顺铂,GP)组(特瑞普利单抗组,n=146)或安慰剂联合化疗组(安慰剂组,n=143)接受治疗,6个周期后分别继续接受特瑞普利单抗(Q3W)或安慰剂单药维持治疗,直至完成2年的治疗、或直至疾病进展、或出现无法耐受的毒性。研究主要终点为独立审查委员会(IRC)根据RECIST v1.1标准评估的意向性分析(ITT)人群的无进展生存期(PFS)。次要终点包括研究者根据RECIST v1.1标准评估的无进展生存期(PFS)、客观缓解率(ORR)、缓解持续时间(DOR)和总生存期(OS)等。
截至2020年5月30日中期分析显示,特瑞普利单抗组的中位治疗持续时间为39周,安慰剂组为36周。与安慰剂组相比,特瑞普利单抗组的PFS显著改善,中位PFS为11.7 vs. 8.0个月(HR = 0.52 [95%CI:0.36-0.74],双侧p = 0.0003)。1年PFS率分别为49.4%和27.9%。在包括PD-L1表达水平亚组在内的所有相关亚组中,均观察到了加予特瑞普利单抗对PFS的改善。特瑞普利单抗组与安慰剂组的ORR为77.4% vs 66.4%(P = 0.033),中位DOR为10.0 vs 5.7个月(HR = 0.50 [95%CI:0.33-0.78],P=0.014)。
截至2021年2月18日,JUPITER-02研究的OS尚未成熟,不过已观察到特瑞普利单抗联合治疗组有总生存的获益趋势,其死亡风险降低了40%。两组的3级及以上不良事件(AE)发生率相似(89.0% vs. 89.5%),特瑞普利单抗组未观察到新的安全性信号。
研究结果显示,与单纯化疗相比,特瑞普利单抗联合GP化疗方案一线治疗复发/转移性鼻咽癌可获得更优的PFS、更高的ORR和更长的DOR,且具有良好的安全性和耐受性。特瑞普利单抗联合GP方案有望成为复发/转移性鼻咽癌一线治疗的新标准。
“与其他一些癌种相比,晚期鼻咽癌的治疗已经处于落后地位,但JUPITER-02研究结果为患者带来了新的改善疗效的希望,也将改变我们对于鼻咽癌的治疗方式。”ASCO首席医学官Julie R. Gralow博士表示。
“鼻咽癌是一种侵袭性强的恶性肿瘤,特别是对于复发/转移性鼻咽癌患者,虽然有含铂化疗作为一线标准方案,但是患者治疗后中位无进展生存期只有7个月左右。JUPITER-02研究的结果令人鼓舞,相较单独应用化疗,特瑞普利单抗联合化疗一线治疗晚期鼻咽癌患者显示出了更优越的疗效和更长的生存获益,且安全性和耐受性良好,有望改写全球复发/转移性鼻咽癌的一线治疗标准。我为我们的中国研究者和本土创新药能够取得这样的成就感到自豪!”中山大学肿瘤防治中心徐瑞华教授表示。
针对鼻咽癌治疗领域,君实生物已在全球范围内布局了“全线贯穿”的特瑞普利单抗单药或联合治疗的临床研究。2021年2月,特瑞普利单抗获得国家药品监督管理局(NMPA)批准,用于既往接受过二线及以上系统治疗失败的复发/转移性鼻咽癌患者的治疗。同月,基于JUPITER-02研究,NMPA还受理了特瑞普利单抗联合化疗用于晚期一线未接受过系统性治疗的复发转移性鼻咽癌的新适应症上市申请。2021年3月,基于美国食品药品监督管理局(FDA)授予的突破性疗法认定,君实生物宣布已开始向FDA滚动提交了特瑞普利单抗用于治疗复发或转移性鼻咽癌的生物制品许可申请(BLA),特瑞普利单抗成为首个向美国FDA提交上市申请的国产抗PD-1单抗。
此外,君实生物在本届ASCO年会上发布的近40项入选摘要中,有多达10项特瑞普利单抗辅助/新辅助/围手术期治疗非小细胞肺癌、食管癌、胃癌、黏膜黑色素瘤等领域的II期研究集中亮相。从后线向前推至一线,乃至辅助/新辅助/围手术期治疗已成为全球范围内肿瘤免疫疗法研究的前沿趋势。
同时,还有多项特瑞普利单抗治疗肝癌、肝内胆管癌(ICC)的最新研究数据也在ASCO年会上亮相。ICC作为君实生物新开拓的研发领域,全球尚无任何III期数据发表。君实生物作为“立足中国”的创新药企,将持续关注和探索胃癌、食管癌、肝胆肿瘤等中国高发癌症领域的临床需求,让更多的中国创新药惠及全球患者。
“鉴于其突出的研究结果,JUPITER-02研究是自从吉西他滨和顺铂化疗被确定为标准治疗以来,在晚期鼻咽癌一线治疗领域首个取得重大治疗进展的全球多中心研究。我们将加快特瑞普利单抗在中国、美国和其他国家的商业化进程,以便将这个令人兴奋的治疗新选择带给更多鼻咽癌患者,”君实生物首席医学官Patricia Keegan博士说。“除了JUPITER-02试验,在ASCO年会期间还将公布特瑞普利单抗的多项其他领域的研究结果,为我们当前的开发策略提供支持。我们已针对多种国内高发的实体瘤,如食管癌、胃癌、肝癌和非小细胞肺癌,及黑色素瘤中亚洲相对高发的黏膜亚型,开展了辅助/新辅助免疫治疗研究。此外,我们也在探索特瑞普利单抗用于肝内胆管癌的治疗方案,目前尚无检查点抑制剂获批用于治疗这个领域。”
参考文献:
- https://gco.iarc.fr/today/data/factsheets/cancers/4-Nasopharynx-fact-sheet.pdf.
- https://gco.iarc.fr/today/data/factsheets/populations/160-china-fact-sheets.pdf.
- Chen YP, et al. Lancet 2019.394:64-80,
- 中国抗癌协会鼻咽癌专业委员会. 中华放射肿瘤学杂志 .2018;27(1):7-15.
- https://ascopubs.org/doi/abs/10.1200/JCO.2020.38.15_suppl.6521.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#瑞普利单抗#
40
#新标准#
42
#ASC#
28
#转移性#
27
学习了
51