J Clin Oncol:预防性脑放疗时避开海马区可在不降低预后的情况下保护认知功能
2021-08-12 Nebula MedSci原创
预防性脑放疗时避开海马区可在不降低预后的情况下保护认知功能
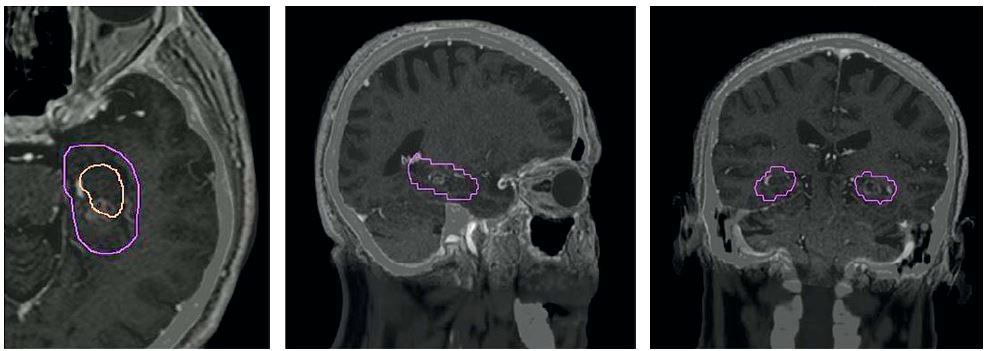
全脑放疗期间,海马神经干细胞接受的辐射剂量与神经认知衰退有关。对于小细胞肺癌 (SCLC) 患者,使用海马回避-预防性颅脑放射治疗 (HA-PCI) 的关键问题是海马回避区内脑转移的发生率。
Randomized Phase III Trial of Prophylactic Cranial Irradiation With or Without Hippocampal Avoidance for Small-Cell Lung Cancer (PREMER): A GICOR-GOECP-SEOR Study
3期GICOR-GOECP-SEOR临床试验,招募了150位SCLC患者(71.3%的患者为限制性疾病),接受标准预防性颅脑放疗(PCI; 25Gy,分10次)或HA-PCI。主要目标是在第3个月时在自由和提示选择性提醒测试 (FCSRT) 中的延迟自由回忆 (DFR);比基线下降≥3分被认为是神经认知功能降低。次要终点包括其他FCSRT评分、生活质量(QoL)、脑转移的发生率和位置以及总体生存期(OS)。分别在基线和PCI后第3、6、12和24个月时评估相关数据。
两组受试者的基线特征平衡良好。存活患者的中位随访时间为40.4个月。与PCI治疗组相比,HA-PCI治疗组从基线到第3个月时的DFR下降较少 (23.5% vs 5.8%;优势比 5;95%CI 1.57-15.86;p=0.003)。
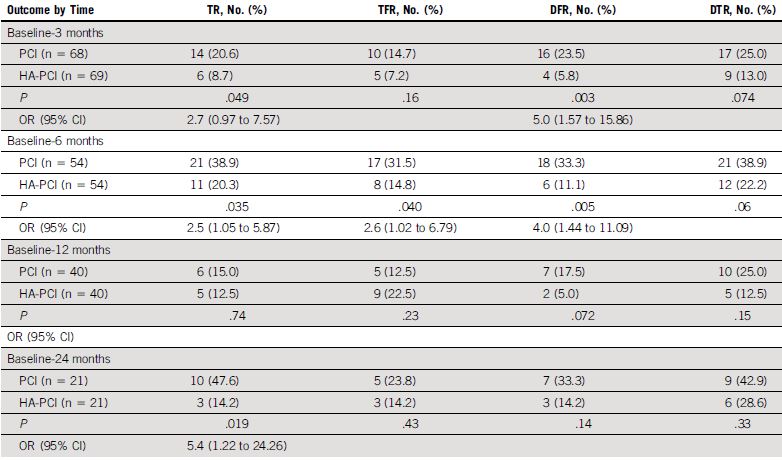
神经认知功能:FCSRT标准化评分较基线相比的降低情况
对所有FCSRT评分的分析显示,与PCI组相比,HA-PCI组第3个月时的总回忆率(TR 8.7% vs 20.6%),第6个月时的DFR(11.1% vs 33.3%)、TR(20.3% vs 38.9%)和总自由回忆(14.8% vs 31.5%),以及第24个月时的TR(14.2% vs 47.6%)下降幅度均更小。
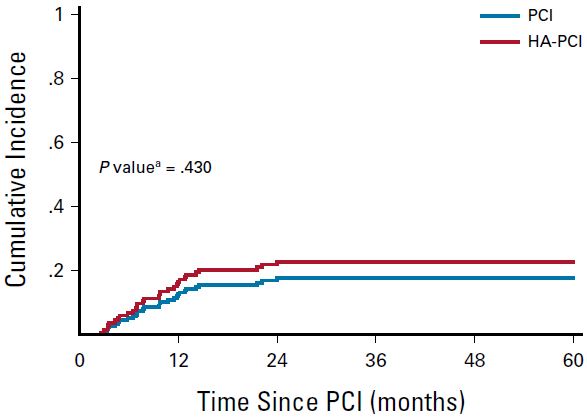
两组患者的脑转移发生率
两组患者的脑转移发生率、OS和QoL均无显著差异。
综上,在PCI期间保留海马体可以更好地保护SCLC患者的认知功能。HA-PCI在脑衰竭、OS和QoL方面与标准PCI没有显著差异。
原始出处:
Núria Rodríguez de Dios, et al. Randomized Phase III Trial of Prophylactic Cranial Irradiation With or Without Hippocampal Avoidance for Small-Cell Lung Cancer (PREMER): A GICOR-GOECP-SEOR Study. Journal of Clinical Oncology. August 11, 2021. https://ascopubs.org/doi/full/10.1200/JCO.21.00639
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Oncol#
42
#预防性#
38
#海马区#
41
谢谢梅斯分享这么多精彩信息
57