Front Onco:基于 MRI 的骨髓放射组学诺模图预测多发性骨髓瘤患者的总生存期
2022-01-01 影像小生 MedSci原创
基于 MRI 的骨髓放射组学可能是预测 MM总体生存期的另一个有用工具。
多发性骨髓瘤(MM)是第二大常见的血液系统恶性肿瘤,以贫血、高钙血症、肾衰竭和溶骨性病变为特征。尽管引入了更有效的治疗方法,这种不治之症的临床结果仍然高度不一致。患者应该接受个性化干预,以获得足够的高质量生活和延长生存期。因此,对于新诊断的MM,需要准确的预后预测标志物来开发合适的治疗方法。
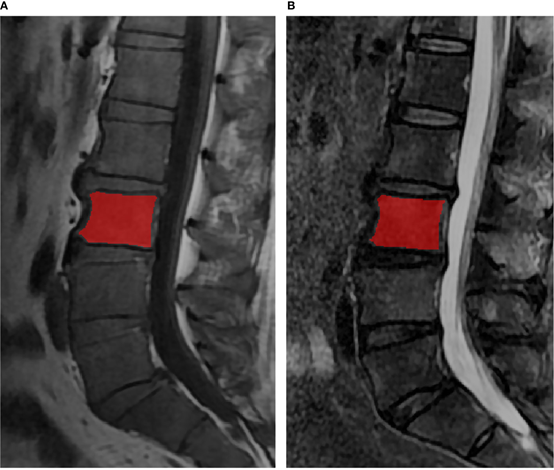
北京大学团队推测骨髓MR放射组学可能为MM患者的生存预测提供增量信息。构建并验证了MM总生存(OS)预测的放射组学诺模图,并将其与其他模型进行比较。此外,还探讨了基于os的放射组学特征与无进展生存期(PFS)之间的潜在相关性。研究结果发表在Radiology杂志。

该研究总共招募了 121 名 MM 患者并分为训练集 (n=84) 和验证集 (n=37)。放射组学特征是由腰椎 MRI 的选定放射组学特征建立的。将放射组学特征和临床危险因素整合到多变量 Cox 回归模型中,以构建放射组学列线图以预测 MM OS。通过一致性指数(C-index)和校准曲线评估列线图的预测能力和准确性,并与临床模型、放射组学特征模型、Durie-Salmon分期系统(DS)和其他四种模型进行比较。国际分期系统 (ISS)。还探讨了放射组学特征与无进展生存期 (PFS) 之间的潜在关联。
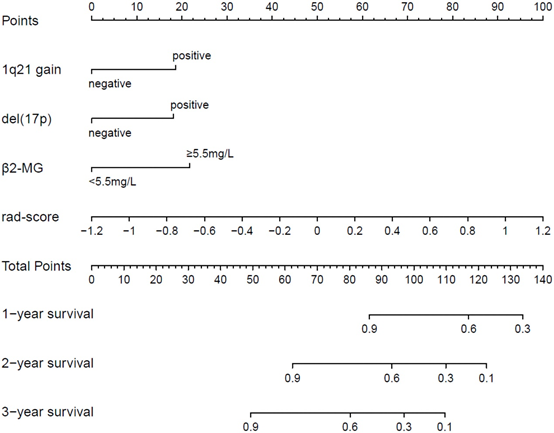
放射组学特征、1q21 增益、del (17p) 和 β2-MG≥5.5 mg/L 与 MM OS 显着相关。
放射组学诺模图的预测能力优于临床模型、放射组学特征模型、DS和ISS(C指数:训练集0.793 vs 0.733 vs 0.742 vs 0.554 vs 0.671 ;验证集中 0.812vs 0.799 vs 0.717vs0.512 vs 0.761)。。
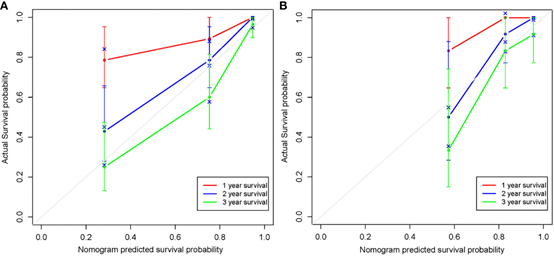
1年、2年和3年生存率接近45度线,表明诺莫图有良好的预测能力。
放射组学特征缺乏 PFS 的预测能力(训练集对数秩P=0.001,验证集中对数秩 P=0.103),而 1 年、2 年和 3 年 PFS 率在高风险组和低风险组之间均显示出显着差异(P≤ 0.05)。

高、低危组无进展生存的Kaplan-Meier分析。(A)训练集中高、低危险组PFS有显著性差异。(B)验证集中高、低风险组PFS无显著差异。
该研究表明,基于MR所建立的放射组学图谱可能具有预测MM OS的能力。此外,基于os的放射组学特征与MM PFS有一定的相关性。这些结果表明骨髓MRI放射组学对MM有一定的预后作用,这种简单的无创方法可能具有临床风险分层的潜力。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#多发性#
33
#生存期#
44
#诺模图#
47
#总生存期#
50