HUMAN BRAIN MAPPING:海洛因成瘾者截断后额-边缘系统神经回路可部分恢复
2022-04-01 MedSci原创 MedSci原创
海洛因成瘾者截断后受损的额-边缘系统神经回路可以部分恢复,这将支持认知能力的提高和渴望的减少。
海洛因成瘾者(HUs)有大脑结构和功能改变。海洛因成瘾是一种复发性脑障碍,几十年来一直是公众和社会关注的一个主要问题。 海洛因作为一种阿片受体激动剂,与GABA能神经元上的μ-阿片受体结合,抑制GABA的抑制作用,并通过增加多巴胺的释放导致奖赏效应的提升。 长期使用海洛因会导致DA系统功能障碍,尤其是前额叶皮层(PFC)和纹状体。然而,人们对长期戒断海洛因后大脑恢复的可能性知之甚少。
Jun Liu等在HUMAN BRAIN MAPPING杂志发表研究文章,调查海洛因成瘾者持久性截断后大脑是否可能恢复。

该研究共有108名海洛因成瘾者完成了结构和功能扫描,其中61人完成了8个月的随访扫描。收集所有参与者的静息状态数据和3D-T1 MR图像,首先在基线(HU1)时,然后在8个月后再次收集(HU2)。认知功能和渴望分别由Trail Making Test-A (TMT-A)和视觉模拟渴望量表测量。分析比较基线和随访时皮层厚度和静息状态功能连接(resting-state functional connectivity, RSFC)差异,得出神经影像学与行为变化之间的相关性。

HU1和HU2的结构差异。HU1:基线时的海洛因戒断使用者。HU2: 8个月随访时海洛因戒断者。
与HU1相比,HU2显示双侧SFG皮质厚度显著增加,左侧距状回、左侧中央后回、左侧梭状回、左侧中央旁回、双侧颞上回、双侧缘上回、右侧中央前回皮质厚度显著降低。
与基线(HU1)相比,HU2认知改善(TMT-A时间缩短),渴望减少,并且在HU2时双侧额上回(SFG)的皮层厚度显著高于HU1。
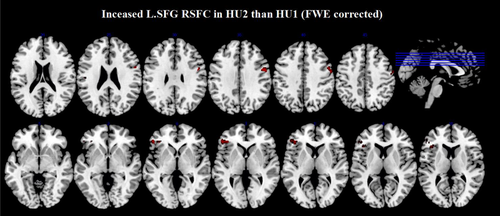
与HU1相比,HU2的左侧SFG-双侧额下回(FWE校正)之间RSFC增加。
HU2时,左SFG与额下回(IFG)、岛叶和伏隔核的RSFC增加,右SFG与IFG、岛叶和眶额皮层(OFC)的RSFC增加。
TMT-A时间的变化与左侧SFG与双侧IFG、双侧尾状核、右侧岛叶的RSFC变化呈负相关。
渴望的改变与左侧OFC-双侧OFC的RSFC变化呈负相关。
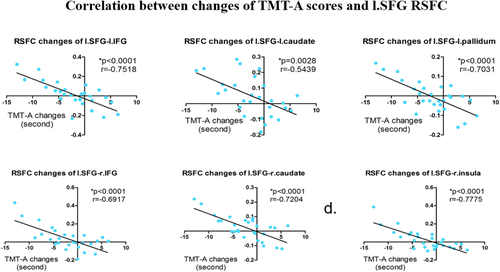
RSFC变化与TMT-A评分的变化呈负相关
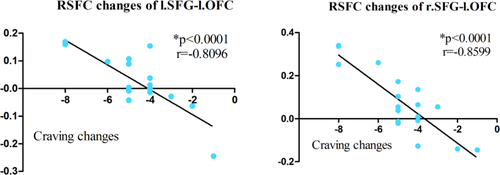
在HUs中,渴望得分的变化与RSFC变化呈负相关
该研究发现在持续性截断后,HUs的认知功能改善,渴望减少,以及SFG皮层厚度增加和SFG RSFC增强。行为改变和神经成像之间的联系进一步暗示了海洛因成瘾者截断后大脑恢复的可能性。
该研究结果表明,海洛因成瘾者截断后受损的额-边缘系统神经回路可以部分恢复,这将支持认知能力的提高和渴望的减少。没有发现右侧SFG RSFC与改善认知功能或减少渴望之间的相关性,这可能是由于大脑的不对称。
原文出处
Recovery of superior frontal gyrus cortical thickness and resting-state functional connectivity in abstinent heroin users after 8 months of follow-up
Wenhan Yang,Min Zhang,Fei Tang,Yanyao Du,Li Fan,Jing Luo,Cui Yan,Shicong Wang,Jun Zhang,Kai Yuan,Jun Liu.First published: 24 March 2022 https://doi.org/10.1002/hbm.25841
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#神经回路#
36
#mapping#
39
#human#
44
#海洛因#
26