Eur Heart J:新的ABC卒中风险评分更有效
2016-03-05 Mechront 译 MedSci原创
<span style="font-family:宋体;mso-ascii-font-family:Calibri; mso-ascii-theme-font:minor-latin;mso-fareast-font-family:宋体;mso-fareast-theme-font: minor-fareast;mso-hansi-font-family:Cal
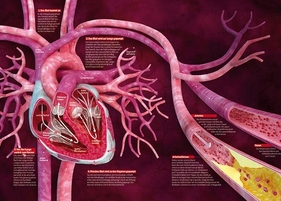
背景:心房颤动(AF)会增加卒中风险。心脏生物标志物的N末端B型利钠肽(NT-proBNP)和心肌肌钙蛋白(cTn-hs)是AF患者卒中风险的独立因素。研究者打算基于生物标志物,开发和验证一种新的风险评分,以改善AF患者卒中的预测。
方法和结果:研究纳入14701名AF患者,检测基线时生物标志物水平,中位数随访1.9年,进行新的风险评分的开发和内部验证。通过Cox回归评估生物标志物和临床变量对卒中的预测,或全身性栓塞的预测,并且每个变量会根据模型系数得到权重比例。接着研究者对1400名AF患者中位数随访3.4年,进行新的风险评分的验证。最重要的预测因素为:既往卒中/短暂性脑缺血发作史、NT-proBNP、cTn-hs和年龄,其中年龄包括在ABC(年龄、生物标志物、临床病史)卒中风险评分中。ABC卒中评分与广泛使用的CHA2DS2-VASc评分相比,在两个队列中ABC评分均具有很好的校准,以及更高的有效性(c-indices:推导队列 0.68 vs. 0.62, P < 0.001;验证队列 0.66 vs. 0.58,P < 0.001)。此外,对于几个重要的亚组进行分析后显示,ABC卒中评分始终如一地提供更高的一致性指数。
结论:ABC卒中评分为当前广泛使用的基于临床的卒中风险评分,可以为AF患者提供更好的决策支持。
原始出处:
Hijazi
Z, Lindbäck J,et al.The ABC (age, biomarkers, clinical history) stroke risk
score: a biomarker-based risk score for predicting stroke in atrial
fibrillation.Eur Heart J. 2016 Feb 25. pii: ehw054.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ABC#
26
#卒中风险#
27
#ART#
26
#HEART#
27